Back
Poster Session A - Sunday Afternoon
A0150 - A Rare Association of Colonic Malakoplakia With Type 2 Diabetes Mellitus
Sunday, October 23, 2022
5:00 PM – 7:00 PM ET
Location: Crown Ballroom

Annie Shergill, MD
Larkin Community Hospital
Fresno, CA
Presenting Author(s)
Award: Presidential Poster Award
Annie Shergill, MD
Larkin Community Hospital, Fresno, CA
Introduction: Malakoplakia is a rare inflammatory, granulomatous disorder that can affect multiple organs such as the brain, adrenal glands, genitourinary and gastrointestinal tracts. The exact pathogenesis is not known but is postulated to be secondary to a macrophage defect resulting in impaired bactericidal activity. Malakoplakia affecting the gastrointestinal tract commonly involves the colon. It is a rare condition and most cases of colonic malakoplakia that have been reported were associated with an underlying immunosuppressive etiology. We present a rare case of colonic malakoplakia in a patient with longstanding history of type 2 diabetes mellitus (T2DM) in the absence of any other previously reported immunosuppressive etiologies.
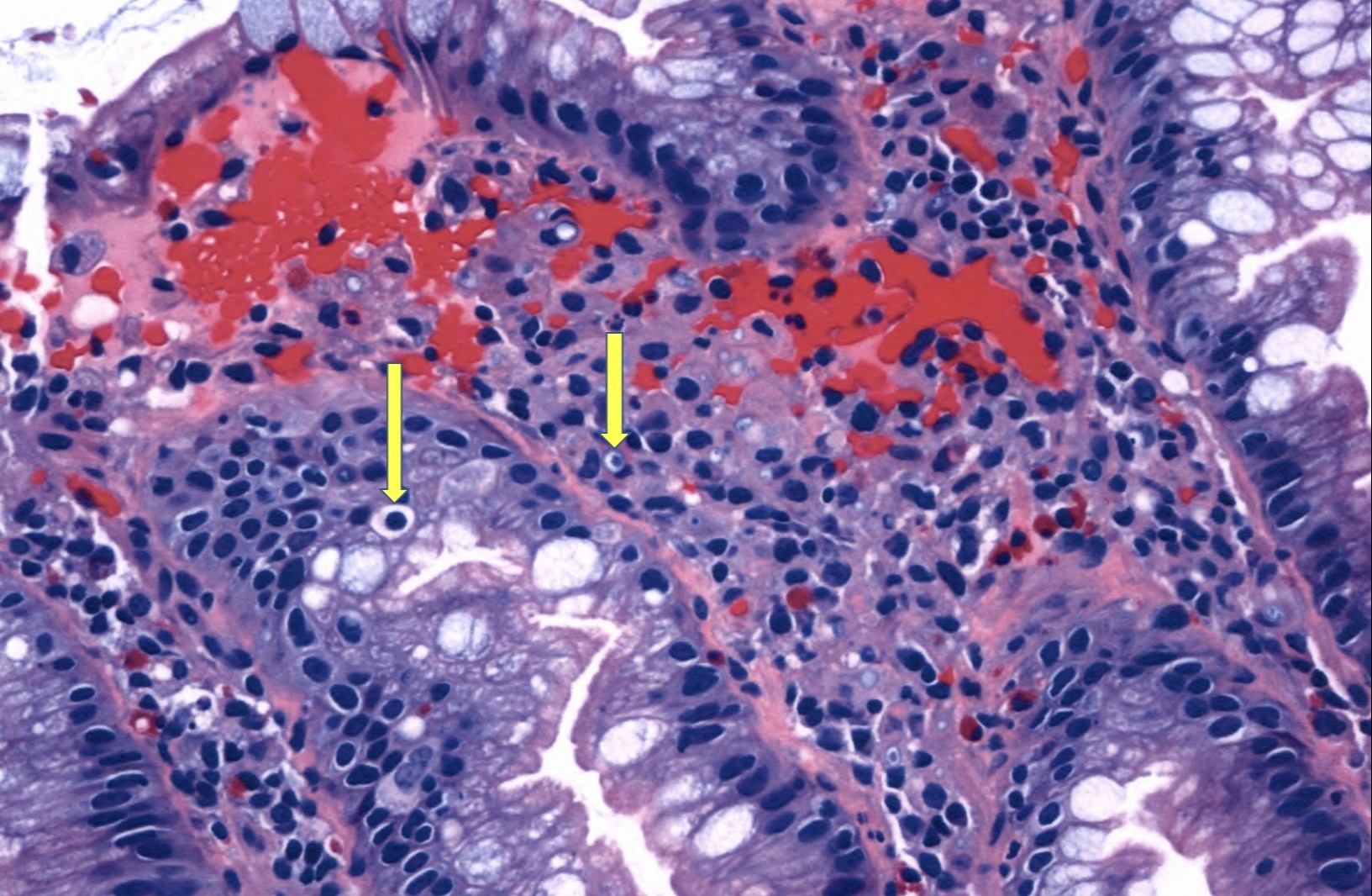
Case Description/Methods: A 54 year old female with past medical history of morbid obesity, dyslipidemia, T2DM for 20 years, hyperplastic colon polyps underwent routine screening colonoscopy. Colonoscopy showed a 6 mm polyp in the cecum which was resected and retrieved. Histopathological examination of the polyp revealed fragments of hyperplastic polyp, macrophage infiltrates with intracytoplasmic inclusions known as Michaelis-Gutmann bodies that are diagnostic of Malakoplakia. Deeper level sections failed to show any evidence of adenoma or sessile serrated lesion. Patient tested negative for Hepatitis B, C and HIV. Age related cancer screening was unremarkable. It was concluded that patient's longstanding history of T2DM rendered her immunocompromised, therefore predisposing her to develop colonic malakoplakia.
Discussion: So far, there are only a few case reports citing malakoplakia of the gastrointestinal tract due to immunocompromised states such as ongoing chemotherapy, post organ transplant recipients, inflammatory bowel disease and lymphoma. We report a unique association of colonic malakoplakia with T2DM and possibly with metabolic syndrome in a patient with morbid obesity and dyslipidemia. We highlight an etiology that has not been thoroughly studied and considering the global prevalence of T2DM, colonic malakoplakia maybe more common and likely goes undiagnosed. It is important to establish an accurate pathological diagnosis of malakoplakia as it may be mistaken for a malignant or premalignant colonic lesion causing unnecessary therapeutic interventions. It is easily treatable with antibiotics such as Bactrim, Rifampin and Fluoroquinolones. Awareness of this rare condition is key in early detection and adequate treatment.
Disclosures:
Annie Shergill, MD. A0150 - A Rare Association of Colonic Malakoplakia With Type 2 Diabetes Mellitus, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
Annie Shergill, MD
Larkin Community Hospital, Fresno, CA
Introduction: Malakoplakia is a rare inflammatory, granulomatous disorder that can affect multiple organs such as the brain, adrenal glands, genitourinary and gastrointestinal tracts. The exact pathogenesis is not known but is postulated to be secondary to a macrophage defect resulting in impaired bactericidal activity. Malakoplakia affecting the gastrointestinal tract commonly involves the colon. It is a rare condition and most cases of colonic malakoplakia that have been reported were associated with an underlying immunosuppressive etiology. We present a rare case of colonic malakoplakia in a patient with longstanding history of type 2 diabetes mellitus (T2DM) in the absence of any other previously reported immunosuppressive etiologies.
Case Description/Methods: A 54 year old female with past medical history of morbid obesity, dyslipidemia, T2DM for 20 years, hyperplastic colon polyps underwent routine screening colonoscopy. Colonoscopy showed a 6 mm polyp in the cecum which was resected and retrieved. Histopathological examination of the polyp revealed fragments of hyperplastic polyp, macrophage infiltrates with intracytoplasmic inclusions known as Michaelis-Gutmann bodies that are diagnostic of Malakoplakia. Deeper level sections failed to show any evidence of adenoma or sessile serrated lesion. Patient tested negative for Hepatitis B, C and HIV. Age related cancer screening was unremarkable. It was concluded that patient's longstanding history of T2DM rendered her immunocompromised, therefore predisposing her to develop colonic malakoplakia.
Discussion: So far, there are only a few case reports citing malakoplakia of the gastrointestinal tract due to immunocompromised states such as ongoing chemotherapy, post organ transplant recipients, inflammatory bowel disease and lymphoma. We report a unique association of colonic malakoplakia with T2DM and possibly with metabolic syndrome in a patient with morbid obesity and dyslipidemia. We highlight an etiology that has not been thoroughly studied and considering the global prevalence of T2DM, colonic malakoplakia maybe more common and likely goes undiagnosed. It is important to establish an accurate pathological diagnosis of malakoplakia as it may be mistaken for a malignant or premalignant colonic lesion causing unnecessary therapeutic interventions. It is easily treatable with antibiotics such as Bactrim, Rifampin and Fluoroquinolones. Awareness of this rare condition is key in early detection and adequate treatment.
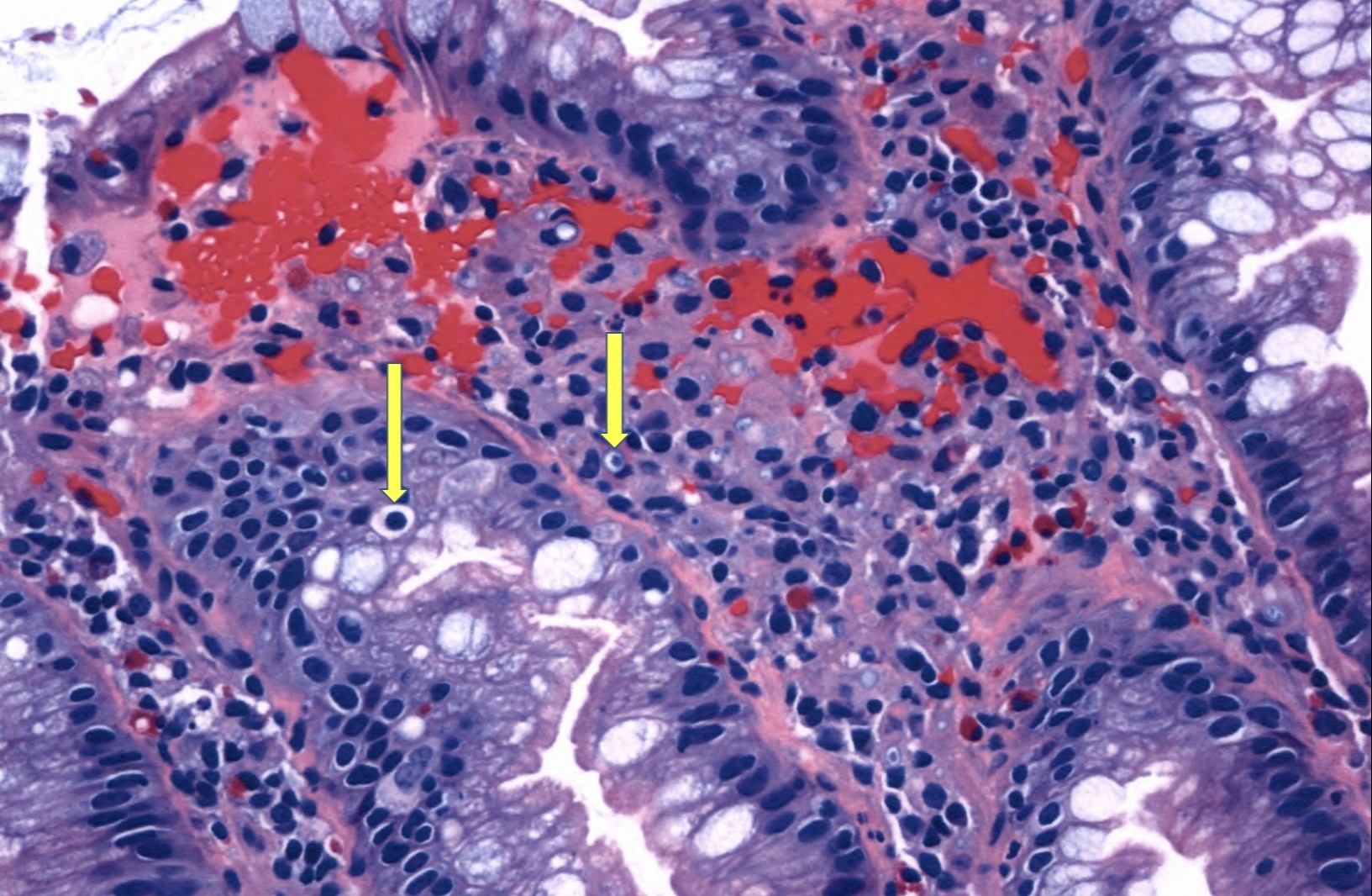
Figure: Cecum polyp: fragments of hyperplastic polyp. Noted within the hyperplastic polyp fragments are macrophage infiltrates with intracytoplasmic Michaelis-Gutmann bodies (yellow arrows) diagnostic of Malakoplakia. Background mixed of non-specific inflammation is also present.
Disclosures:
Annie Shergill indicated no relevant financial relationships.
Annie Shergill, MD. A0150 - A Rare Association of Colonic Malakoplakia With Type 2 Diabetes Mellitus, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.

