Back
Poster Session A - Sunday Afternoon
A0066 - Silent Hemoperitoneum and MRSA Bacterascites: An Unusual Presentation of Gallbladder Perforation
Sunday, October 23, 2022
5:00 PM – 7:00 PM ET
Location: Crown Ballroom

Kuntal Bhowmick, MD
Brown University
Providence, RI
Presenting Author(s)
Kuntal Bhowmick, MD, Breton Roussel, MD, Sean Fine, MD, MS
Brown University, Providence, RI
Introduction: Gallbladder perforation (GBP) is an uncommon, life-threatening event, most often seen as a complication of acute cholecystitis. Occurrence of GBP in the absence of cholecystitis is exceedingly rare, but may occur in those with cholelithiasis. We report a case of spontaneous GBP without cholecystitis presenting as painless hemoperitoneum and methicillin-resistant Staphylococcal aureus (MRSA) bacterascites in a patient with decompensated cirrhosis.
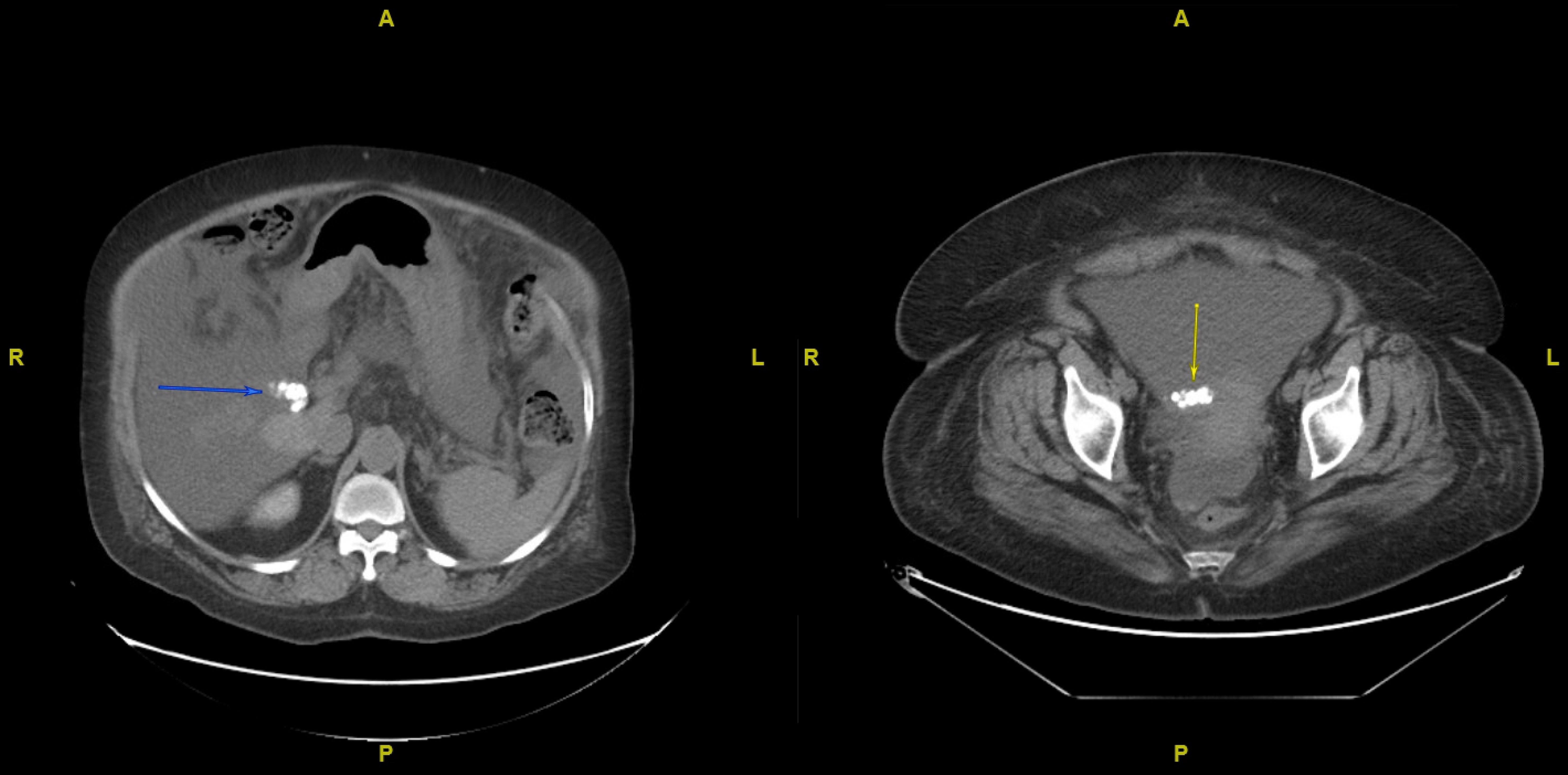
Case Description/Methods: A 63 year old female with past history of NASH cirrhosis (MELD 27, Child-Pugh C), esophageal varices, and ascites requiring weekly therapeutic paracentesis presented with encephalopathy. A paracentesis on admission was negative for spontaneous bacterial peritonitis by cell count and culture. CT imaging on admission revealed a partial small bowel obstruction (pSBO) and cholelithiasis with an otherwise normal gallbladder and biliary tree. The pSBO resolved with conservative management. One week into the hospitalization, her ascites worsened. A second paracentesis showed 253,290 RBC/mm3, with a corrected ANC of -54 cells/mm3. A 3 gram serum hemoglobin drop was also noted. A repeat abdominal CT scan showed a non-inflamed gallbladder with her known gallstones now layering in the pelvis, suggestive of GBP (figure 1). She was initially started on piperacillin-tazobactam, but her ascitic fluid culture later grew MRSA. Based on her surgical risk and overall clinical stability, she was managed non-operatively. She was transitioned to indefinite therapy with amoxicillin-clavulanate and doxycycline, and later discharged home.
Discussion: Most GBPs are due to severe inflammation or trauma. Risk factors for spontaneous GBP include cholelithiasis, congenital obstruction, and anticoagulant therapy. Although rare, patients with cirrhosis may have a higher risk for GBP due to venous congestion from portal hypertension and their propensity for cholelithiasis. Her MRSA bacterascites may have been from iatrogenic seeding during the first paracentesis, but the timeline to discovery raised concerns that it originated from the GBP. MRSA is rarely a biliary pathogen, but may result from bacteremia that seeds the gallbladder. Regardless, the patient began indefinite antibiotic therapy, as her gallstones posed as persistent nidi for infection. This case highlights the rare possibility of silent GBP as a cause for worsening ascites, as well as the therapeutic dilemma of retained peritoneal gallstones in a poor surgical candidate.
Disclosures:
Kuntal Bhowmick, MD, Breton Roussel, MD, Sean Fine, MD, MS. A0066 - Silent Hemoperitoneum and MRSA Bacterascites: An Unusual Presentation of Gallbladder Perforation, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
Brown University, Providence, RI
Introduction: Gallbladder perforation (GBP) is an uncommon, life-threatening event, most often seen as a complication of acute cholecystitis. Occurrence of GBP in the absence of cholecystitis is exceedingly rare, but may occur in those with cholelithiasis. We report a case of spontaneous GBP without cholecystitis presenting as painless hemoperitoneum and methicillin-resistant Staphylococcal aureus (MRSA) bacterascites in a patient with decompensated cirrhosis.
Case Description/Methods: A 63 year old female with past history of NASH cirrhosis (MELD 27, Child-Pugh C), esophageal varices, and ascites requiring weekly therapeutic paracentesis presented with encephalopathy. A paracentesis on admission was negative for spontaneous bacterial peritonitis by cell count and culture. CT imaging on admission revealed a partial small bowel obstruction (pSBO) and cholelithiasis with an otherwise normal gallbladder and biliary tree. The pSBO resolved with conservative management. One week into the hospitalization, her ascites worsened. A second paracentesis showed 253,290 RBC/mm3, with a corrected ANC of -54 cells/mm3. A 3 gram serum hemoglobin drop was also noted. A repeat abdominal CT scan showed a non-inflamed gallbladder with her known gallstones now layering in the pelvis, suggestive of GBP (figure 1). She was initially started on piperacillin-tazobactam, but her ascitic fluid culture later grew MRSA. Based on her surgical risk and overall clinical stability, she was managed non-operatively. She was transitioned to indefinite therapy with amoxicillin-clavulanate and doxycycline, and later discharged home.
Discussion: Most GBPs are due to severe inflammation or trauma. Risk factors for spontaneous GBP include cholelithiasis, congenital obstruction, and anticoagulant therapy. Although rare, patients with cirrhosis may have a higher risk for GBP due to venous congestion from portal hypertension and their propensity for cholelithiasis. Her MRSA bacterascites may have been from iatrogenic seeding during the first paracentesis, but the timeline to discovery raised concerns that it originated from the GBP. MRSA is rarely a biliary pathogen, but may result from bacteremia that seeds the gallbladder. Regardless, the patient began indefinite antibiotic therapy, as her gallstones posed as persistent nidi for infection. This case highlights the rare possibility of silent GBP as a cause for worsening ascites, as well as the therapeutic dilemma of retained peritoneal gallstones in a poor surgical candidate.
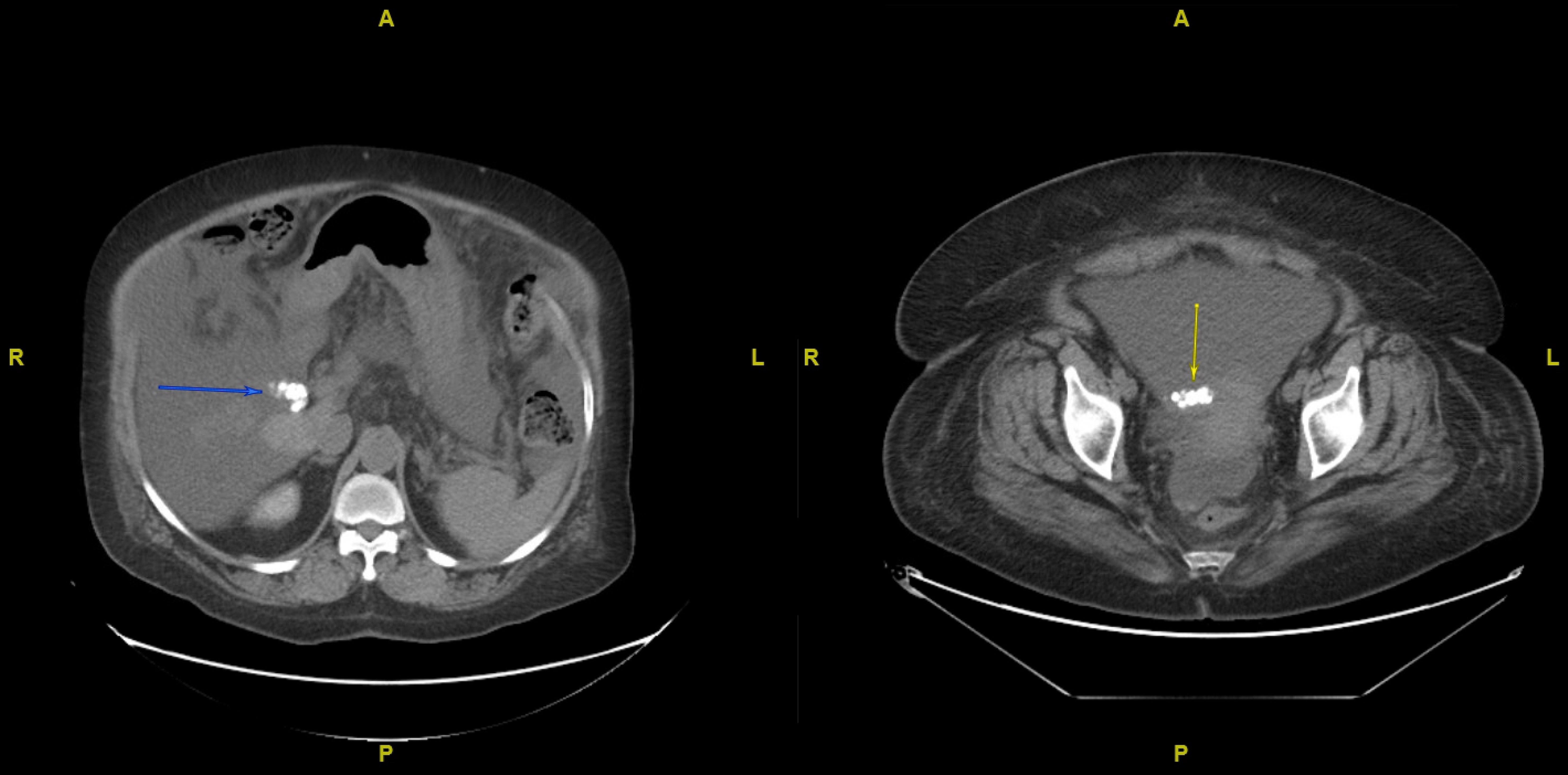
Figure: Gallstones residing in intact gallbladder on left, compared to subsequent scan on the right demonstrating gallstones in patient's pelvis.
Disclosures:
Kuntal Bhowmick indicated no relevant financial relationships.
Breton Roussel indicated no relevant financial relationships.
Sean Fine: Bristol Meyers Squibb – Consultant.
Kuntal Bhowmick, MD, Breton Roussel, MD, Sean Fine, MD, MS. A0066 - Silent Hemoperitoneum and MRSA Bacterascites: An Unusual Presentation of Gallbladder Perforation, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
