Back
Poster Session A - Sunday Afternoon
A0053 - Two Cases of Post-COVID Cholangiopathy: A Rare Complication of SARS-CoV-2 Infection
Sunday, October 23, 2022
5:00 PM – 7:00 PM ET
Location: Crown Ballroom
.jpg)
Hamza I. Khan, MD
University of Texas Health Science Center
San Antonio, TX
Presenting Author(s)
Hamza I. Khan, MD1, Nagasri Shankar, MD2, Venkata Katabathina, MD2, Chandraprakash Umapathy, MD3, Juan Echavarria, MS, MD3, Fabian Rodas-Ochoa, MD3
1University of Texas Health Science Center, San Antonio, TX; 2UT Health San Antonio, San Antonio, TX; 3University of Texas Health San Antonio, San Antonio, TX
Introduction: Hepatobiliary manifestations are seen in most SARS-CoV-2 infections as mild hepatocellular elevations. A rare complication of severe SARS-CoV-2 infection, termed post-COVID cholangiopathy, has been reported a handful of times. Herein, we present two unique cases of post-COVID cholangiopathy to offer further insight into this unique entity.
Case Description/Methods: Patient 1 is a 69-year-old Hispanic female with a past medical history of prior drug-induced liver injury admitted in August 2020 for acute hypoxic respiratory failure secondary to SARS-CoV-2 pneumonia requiring mechanical ventilation and vasopressor support. 390 days following initial admission, the patient was found to have an elevated alkaline phosphatase (ALP,985 U/L), gamma-glutamyl transferase (GGT, >1600 units), and normal total bilirubin (TBILI, 0.4 mg/dl). Magnetic resonance cholangiopancreatography (MRCP) showed intrahepatic biliary ductal dilatations. The patient continues to follow with hepatology with a most recent MELD of 6.
Patient 2 is a 27-year-old Hispanic male with chronic kidney disease admitted in August 2021 for provoked seizures in the setting of active SARS-CoV-2 infection. The patient rapidly deteriorated requiring mechanical ventilation, vasopressors, and continuous renal replacement therapy. On day 49 of admission laboratory values revealed an elevated TBILI (31.6 mg/dl), GGT (1569 U/L), and ALP (5000 U/L). On day 79, a liver biopsy showed signs of large duct obstruction. MRCP on day 139 showed intrahepatic biliary strictures and dilatation not seen on prior MRCP. The patient was unable to undergo liver transplant evaluation despite a MELD of 36.
Discussion: The most striking features of post-COVID cholangiopathy are the disproportionate elevation in ALP followed by delayed intrahepatic biliary strictures and dilatations. Post-COVID cholangiopathy has exclusively been reported in patients requiring ventilation and vasopressor support. As such, it is postulated that this disease is a result of biliary ischemia induced by COVID hypoxemia and vasopressor-induced splanchnic hypoperfusion. Although rare, we believe the high mortality rate of severe SARS-CoV-2 infection and the delayed histological and anatomical findings needed for diagnosis have contributed to an underestimation of the prevalence of post-COVID cholangiopathy. Further studies are needed to establish the true prevalence as well as definitive diagnostic and treatment criteria for this novel disease.
Disclosures:
Hamza I. Khan, MD1, Nagasri Shankar, MD2, Venkata Katabathina, MD2, Chandraprakash Umapathy, MD3, Juan Echavarria, MS, MD3, Fabian Rodas-Ochoa, MD3. A0053 - Two Cases of Post-COVID Cholangiopathy: A Rare Complication of SARS-CoV-2 Infection, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1University of Texas Health Science Center, San Antonio, TX; 2UT Health San Antonio, San Antonio, TX; 3University of Texas Health San Antonio, San Antonio, TX
Introduction: Hepatobiliary manifestations are seen in most SARS-CoV-2 infections as mild hepatocellular elevations. A rare complication of severe SARS-CoV-2 infection, termed post-COVID cholangiopathy, has been reported a handful of times. Herein, we present two unique cases of post-COVID cholangiopathy to offer further insight into this unique entity.
Case Description/Methods: Patient 1 is a 69-year-old Hispanic female with a past medical history of prior drug-induced liver injury admitted in August 2020 for acute hypoxic respiratory failure secondary to SARS-CoV-2 pneumonia requiring mechanical ventilation and vasopressor support. 390 days following initial admission, the patient was found to have an elevated alkaline phosphatase (ALP,985 U/L), gamma-glutamyl transferase (GGT, >1600 units), and normal total bilirubin (TBILI, 0.4 mg/dl). Magnetic resonance cholangiopancreatography (MRCP) showed intrahepatic biliary ductal dilatations. The patient continues to follow with hepatology with a most recent MELD of 6.
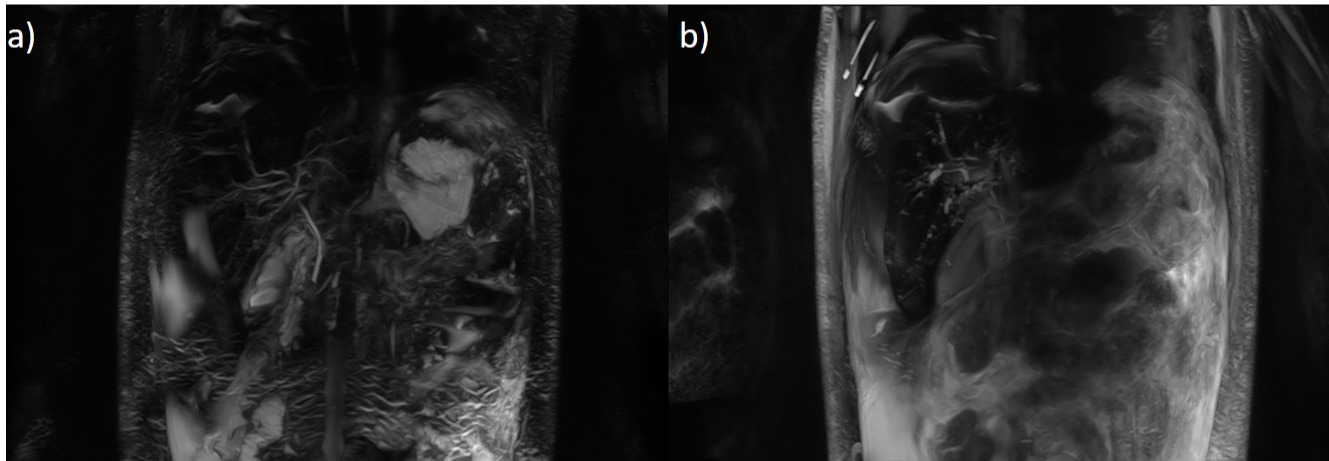
Patient 2 is a 27-year-old Hispanic male with chronic kidney disease admitted in August 2021 for provoked seizures in the setting of active SARS-CoV-2 infection. The patient rapidly deteriorated requiring mechanical ventilation, vasopressors, and continuous renal replacement therapy. On day 49 of admission laboratory values revealed an elevated TBILI (31.6 mg/dl), GGT (1569 U/L), and ALP (5000 U/L). On day 79, a liver biopsy showed signs of large duct obstruction. MRCP on day 139 showed intrahepatic biliary strictures and dilatation not seen on prior MRCP. The patient was unable to undergo liver transplant evaluation despite a MELD of 36.
Discussion: The most striking features of post-COVID cholangiopathy are the disproportionate elevation in ALP followed by delayed intrahepatic biliary strictures and dilatations. Post-COVID cholangiopathy has exclusively been reported in patients requiring ventilation and vasopressor support. As such, it is postulated that this disease is a result of biliary ischemia induced by COVID hypoxemia and vasopressor-induced splanchnic hypoperfusion. Although rare, we believe the high mortality rate of severe SARS-CoV-2 infection and the delayed histological and anatomical findings needed for diagnosis have contributed to an underestimation of the prevalence of post-COVID cholangiopathy. Further studies are needed to establish the true prevalence as well as definitive diagnostic and treatment criteria for this novel disease.
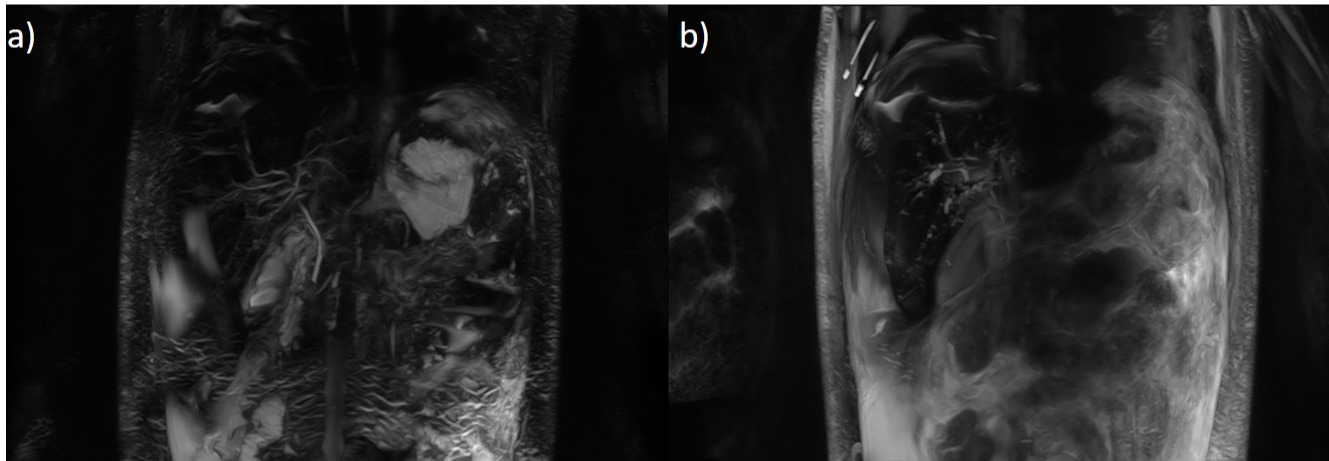
Figure: Patient 2 MRCP day 49 (A) vs day 139 (B).
Disclosures:
Hamza Khan indicated no relevant financial relationships.
Nagasri Shankar indicated no relevant financial relationships.
Venkata Katabathina indicated no relevant financial relationships.
Chandraprakash Umapathy indicated no relevant financial relationships.
Juan Echavarria indicated no relevant financial relationships.
Fabian Rodas-Ochoa indicated no relevant financial relationships.
Hamza I. Khan, MD1, Nagasri Shankar, MD2, Venkata Katabathina, MD2, Chandraprakash Umapathy, MD3, Juan Echavarria, MS, MD3, Fabian Rodas-Ochoa, MD3. A0053 - Two Cases of Post-COVID Cholangiopathy: A Rare Complication of SARS-CoV-2 Infection, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
