Back
Poster Session A - Sunday Afternoon
Category: Liver
A0498 - Evaluation of Elevated Liver Enzymes in Hospitalized Patients – A Quality Improvement Project
Sunday, October 23, 2022
5:00 PM – 7:00 PM ET
Location: Crown Ballroom
- AK
Ali Khalifa, MD
Rutgers Medical School of Robert Wood Johnson - Saint Peter's University Hospital
New Brunswick, New Jersey
Presenting Author(s)
Ali Khalifa, MD1, Sotirios Doukas, MD2, Masha Osman, MS3, Arkady Broder, MD, FACG4
1Rutgers Medical School of Robert Wood Johnson - Saint Peter's University Hospital, New Brunswick, NJ; 2Rutgers Robert Wood Johnson Medical School/Saint Peter's University Hospital, New Brunswick, NJ; 3Rutgers-Robert Wood Johnson Medical School/Saint Peter's University Hospital, New Brunswick, NJ; 4Rutgers Medical School of Robert Wood Johnson, Saint Peter's University Hospital, New Brunswick, NJ
Introduction: Clinicians are required to assess abnormal liver chemistries on a daily basis. The ACG provides clear specific recommendations in management of patients admitted for elevated liver enzymes (LEs). We here aimed to evaluate to the current hospital practice in evaluation of elevated LEs and to highlight how we may further incorporate the appropriate guidance to provide evidence-based care.
Methods: We retrospectively identified 50 patients consecutively admitted for elevated LEs between 1/2021 and 1/2022 (utilizing ICD code R74.01). We focused our analysis on patients with moderate (5-15X ULN) and severe ( >15X ULN) elevation in LEs since inpatient workup is highly recommended in these patients. The current ACG guidelines recommend the following tests in these patients: HAV IgM, HAV IgG, HBsAg, HBcAb IgM, HBcAb IgG, HBsAb, HCV Ab with PCR confirmation if positive, HSV, EBV, CMV, ceruloplasmin, iron panel, ANA, ASMA, Anti-LKM, IgG, serum drug and urine toxicology panels, and doppler abdominal ultrasound.
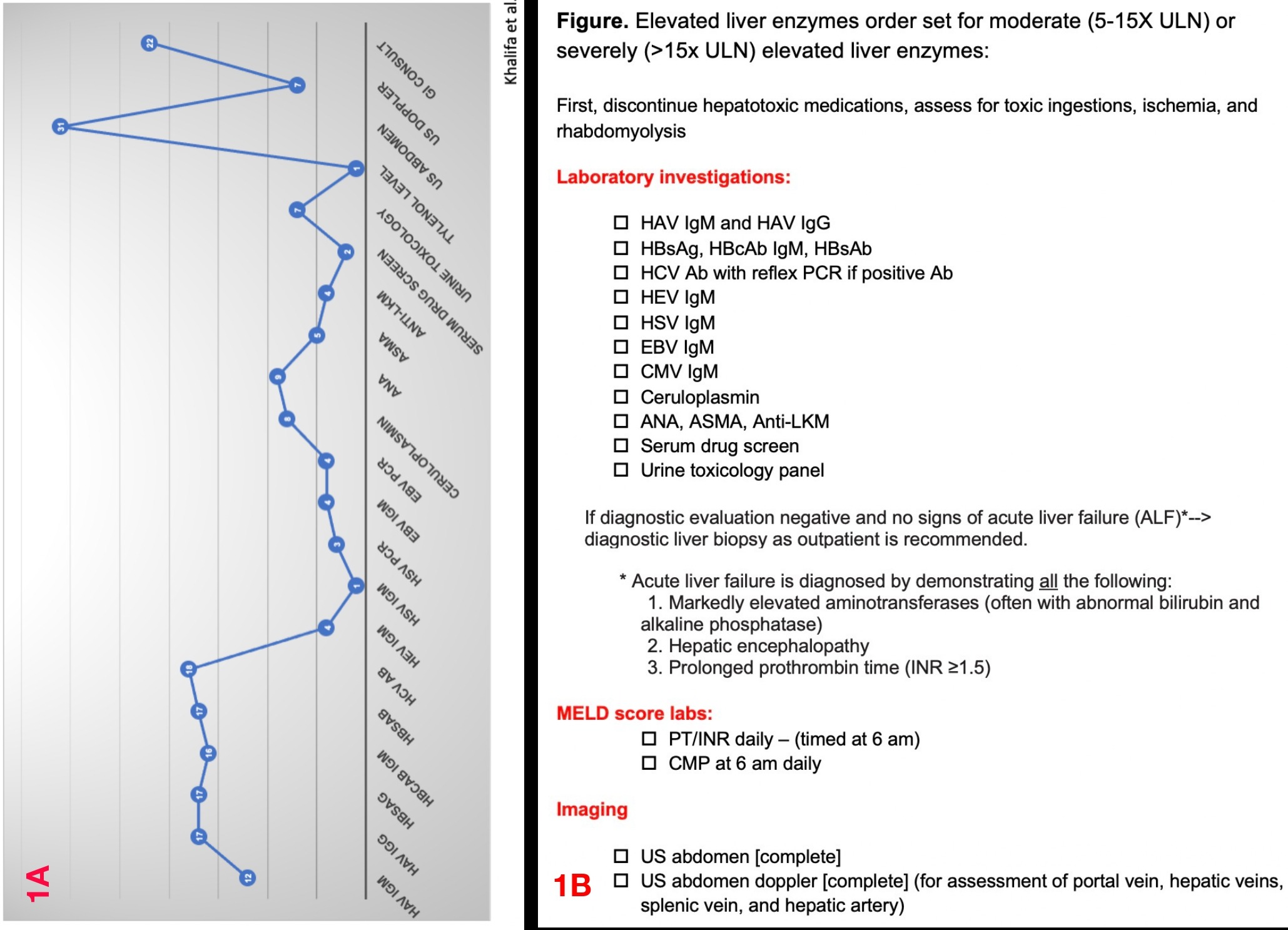
Results: In the 50 patients admitted for elevated LEs, 30 patients were men, and the majority were White (35 patients). The mean age of the cohort was 50±11 years. The mean and SD of liver tests were: ALT 338±336 U/L, AST 329±330 U/L, ALP 253±254 U/L, bilirubin 5.2±8.7 mg/dL, and INR 1.2±1.3. Overall, a complete workup for the elevated liver enzymes was performed in 12/50 patients only (24%) (Figure 1A). Among the 33 patients who had “moderate” or “severe” elevations of LEs, the average number of tests and imaging studies ordered for each patient was 7/24 only (29%). Furthermore, complete evaluation, based on the ACG recommendation, was not performed at admission in any of the patients. After initial workup, a defined diagnosis was documented in 19/33 patients (58%). Gastroenterology (GI) consultation was requested in 21/33 patients (2/3rds). In 16/21 (76%) patients where GI was consulted, the diagnosis was established only after GI recommended further investigations based on the ACG guidelines. Length of stay was 2.6±2.7 days.
Discussion: Our data suggest that in most of the patients the proper workup has been incomplete or delayed which may have prolonged the length of hospital stay and cost of care. Thus, we recommended education of the medical team on the existing guidelines (including consulting gastroenterology specialist) as well as incorporation of the recommendations in a proper order set to improve clinician efficiency and provide decision-making guidance (Figure 1B).
Disclosures:
Ali Khalifa, MD1, Sotirios Doukas, MD2, Masha Osman, MS3, Arkady Broder, MD, FACG4. A0498 - Evaluation of Elevated Liver Enzymes in Hospitalized Patients – A Quality Improvement Project, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1Rutgers Medical School of Robert Wood Johnson - Saint Peter's University Hospital, New Brunswick, NJ; 2Rutgers Robert Wood Johnson Medical School/Saint Peter's University Hospital, New Brunswick, NJ; 3Rutgers-Robert Wood Johnson Medical School/Saint Peter's University Hospital, New Brunswick, NJ; 4Rutgers Medical School of Robert Wood Johnson, Saint Peter's University Hospital, New Brunswick, NJ
Introduction: Clinicians are required to assess abnormal liver chemistries on a daily basis. The ACG provides clear specific recommendations in management of patients admitted for elevated liver enzymes (LEs). We here aimed to evaluate to the current hospital practice in evaluation of elevated LEs and to highlight how we may further incorporate the appropriate guidance to provide evidence-based care.
Methods: We retrospectively identified 50 patients consecutively admitted for elevated LEs between 1/2021 and 1/2022 (utilizing ICD code R74.01). We focused our analysis on patients with moderate (5-15X ULN) and severe ( >15X ULN) elevation in LEs since inpatient workup is highly recommended in these patients. The current ACG guidelines recommend the following tests in these patients: HAV IgM, HAV IgG, HBsAg, HBcAb IgM, HBcAb IgG, HBsAb, HCV Ab with PCR confirmation if positive, HSV, EBV, CMV, ceruloplasmin, iron panel, ANA, ASMA, Anti-LKM, IgG, serum drug and urine toxicology panels, and doppler abdominal ultrasound.
Results: In the 50 patients admitted for elevated LEs, 30 patients were men, and the majority were White (35 patients). The mean age of the cohort was 50±11 years. The mean and SD of liver tests were: ALT 338±336 U/L, AST 329±330 U/L, ALP 253±254 U/L, bilirubin 5.2±8.7 mg/dL, and INR 1.2±1.3. Overall, a complete workup for the elevated liver enzymes was performed in 12/50 patients only (24%) (Figure 1A). Among the 33 patients who had “moderate” or “severe” elevations of LEs, the average number of tests and imaging studies ordered for each patient was 7/24 only (29%). Furthermore, complete evaluation, based on the ACG recommendation, was not performed at admission in any of the patients. After initial workup, a defined diagnosis was documented in 19/33 patients (58%). Gastroenterology (GI) consultation was requested in 21/33 patients (2/3rds). In 16/21 (76%) patients where GI was consulted, the diagnosis was established only after GI recommended further investigations based on the ACG guidelines. Length of stay was 2.6±2.7 days.
Discussion: Our data suggest that in most of the patients the proper workup has been incomplete or delayed which may have prolonged the length of hospital stay and cost of care. Thus, we recommended education of the medical team on the existing guidelines (including consulting gastroenterology specialist) as well as incorporation of the recommendations in a proper order set to improve clinician efficiency and provide decision-making guidance (Figure 1B).
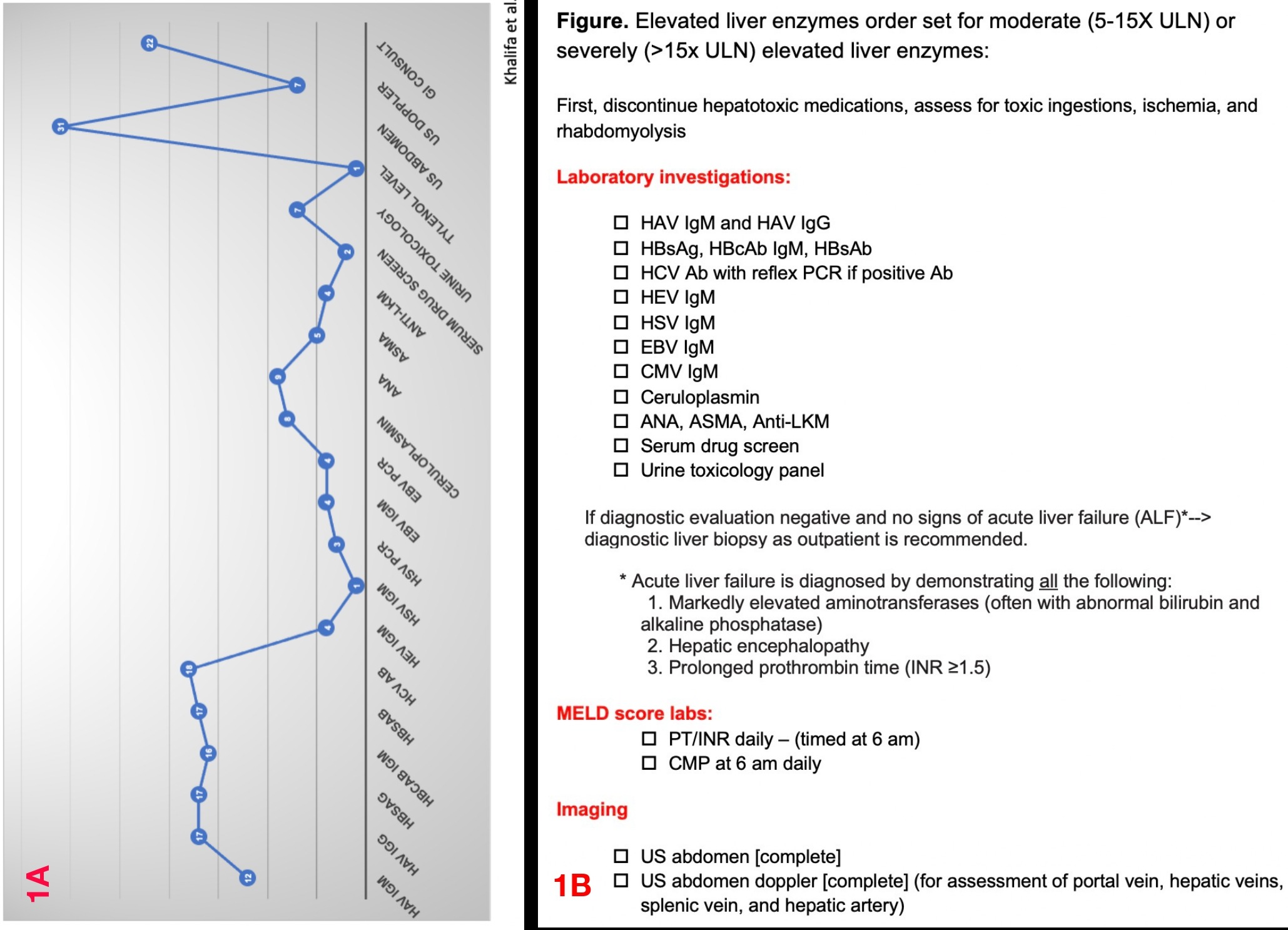
Figure: Figure1A. Laboratory tests and imaging studies ordered for the study cohort (50 patients)
Figure 1B. Elevated liver enzymes order set for moderate (5-15X ULN) or severely (>15x ULN) elevated liver enzymes
Figure 1B. Elevated liver enzymes order set for moderate (5-15X ULN) or severely (>15x ULN) elevated liver enzymes
Disclosures:
Ali Khalifa indicated no relevant financial relationships.
Sotirios Doukas indicated no relevant financial relationships.
Masha Osman indicated no relevant financial relationships.
Arkady Broder: GITrak – Advisory Committee/Board Member.
Ali Khalifa, MD1, Sotirios Doukas, MD2, Masha Osman, MS3, Arkady Broder, MD, FACG4. A0498 - Evaluation of Elevated Liver Enzymes in Hospitalized Patients – A Quality Improvement Project, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
