Back

Poster Session A - Sunday Afternoon
Category: IBD
A0332 - Obesity as a Prognostic Factor for Colonic Resection in Patients With Ulcerative Colitis: Insights From the National Inpatient Sample
Sunday, October 23, 2022
5:00 PM – 7:00 PM ET
Location: Crown Ballroom
Has Audio
Laine A. Lyles, DO
Prisma Health-Midlands/ University of South Carolina
Lexington, SC
Presenting Author(s)
Laine A. Lyles, DO1, Eric Klingeman, DO2, James Laney, 3, Reagan Farmer, 3, M. Clay O'Brien, BS3, Victoria Sanderford, 4, William E. Lyles, MD, FACG5
1Prisma Health-Midlands/ University of South Carolina, Lexington, SC; 2University of South Carolina, Lexington, SC; 3University of South Carolina School of Medicine, Columbia, SC; 4University of South Carolina School of Medicine Columbia, Columbia, SC; 5Blount Memorial Physicians Group, Rockford, TN
Introduction: In ulcerative colitis (UC), there are several biologic and lifestyle factors that are associated with development and progression of disease. Poorly controlled UC often results in colectomy, frequently with high rates of postoperative complications. Previous research has suggested a relationship between obesity and UC prognosis in certain areas, but a potential relationship between obesity and need for colonic resections has not been established.
Methods: This is a retrospective cohort study using the 2019 National Inpatient Sample (NIS). Inclusion criteria were a principal diagnosis of UC and age >18. The patients were divided into two groups: obese and nonobese based on a secondary diagnosis of obesity. The primary outcome was the rate of colonic resection. Secondary outcomes were: 1) mortality 2) underwent colonoscopy 3) length of stay 4) total hospital charges. Confounders were adjusted for using multivariate regression analysis of the following variables: sex, income, race, insurance, Charlson comorbidity index (CCI), hospital bedsize, location, teaching status, and region
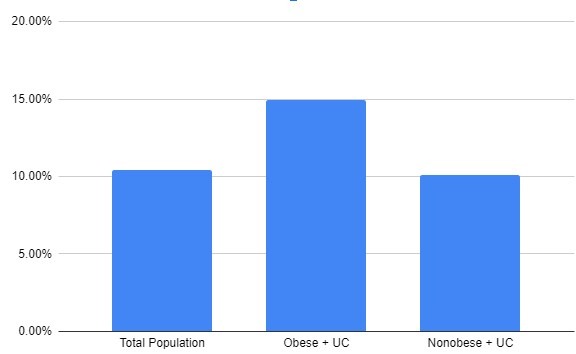
Results: 34,490 Patients were included in the study, 7.26% of which were obese. Both obese and nonobese groups predominantly consisted of Caucasian females with a CCI of 0 who were treated at large, urban teaching hospitals in the Southern United States. The mean age of the total population was 49.6. For the total patient population studied, 37.51% required a colonoscopy and 10.4% required resection. Compared to the rate of resection in patients without obesity, those with UC and obesity had a 70% increase in odds of colonic resection when compared to non obese patients while adjusting for confounders. Secondary outcomes showed no statistically significant differences between the two groups.
Discussion: Obesity continues to pose a significant challenge to healthcare providers, as it creates strain on hospitals while also increasing likelihood of detrimental sequelae. This study demonstrates that individuals admitted with a primary diagnosis of ulcerative colitis, who are also obese are at increased risk of undergoing colonic resection. Based on these results, obesity acts as a negative prognostic factor in the disease process of UC and should enter into discussion that all physicians have with their patients upon initial diagnosis of UC. Studies have found that rates of obesity are increasing amongst the population diagnosed with UC, making this discussion even more crucial to guiding care.
Disclosures:
Laine A. Lyles, DO1, Eric Klingeman, DO2, James Laney, 3, Reagan Farmer, 3, M. Clay O'Brien, BS3, Victoria Sanderford, 4, William E. Lyles, MD, FACG5. A0332 - Obesity as a Prognostic Factor for Colonic Resection in Patients With Ulcerative Colitis: Insights From the National Inpatient Sample, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1Prisma Health-Midlands/ University of South Carolina, Lexington, SC; 2University of South Carolina, Lexington, SC; 3University of South Carolina School of Medicine, Columbia, SC; 4University of South Carolina School of Medicine Columbia, Columbia, SC; 5Blount Memorial Physicians Group, Rockford, TN
Introduction: In ulcerative colitis (UC), there are several biologic and lifestyle factors that are associated with development and progression of disease. Poorly controlled UC often results in colectomy, frequently with high rates of postoperative complications. Previous research has suggested a relationship between obesity and UC prognosis in certain areas, but a potential relationship between obesity and need for colonic resections has not been established.
Methods: This is a retrospective cohort study using the 2019 National Inpatient Sample (NIS). Inclusion criteria were a principal diagnosis of UC and age >18. The patients were divided into two groups: obese and nonobese based on a secondary diagnosis of obesity. The primary outcome was the rate of colonic resection. Secondary outcomes were: 1) mortality 2) underwent colonoscopy 3) length of stay 4) total hospital charges. Confounders were adjusted for using multivariate regression analysis of the following variables: sex, income, race, insurance, Charlson comorbidity index (CCI), hospital bedsize, location, teaching status, and region
Results: 34,490 Patients were included in the study, 7.26% of which were obese. Both obese and nonobese groups predominantly consisted of Caucasian females with a CCI of 0 who were treated at large, urban teaching hospitals in the Southern United States. The mean age of the total population was 49.6. For the total patient population studied, 37.51% required a colonoscopy and 10.4% required resection. Compared to the rate of resection in patients without obesity, those with UC and obesity had a 70% increase in odds of colonic resection when compared to non obese patients while adjusting for confounders. Secondary outcomes showed no statistically significant differences between the two groups.
Discussion: Obesity continues to pose a significant challenge to healthcare providers, as it creates strain on hospitals while also increasing likelihood of detrimental sequelae. This study demonstrates that individuals admitted with a primary diagnosis of ulcerative colitis, who are also obese are at increased risk of undergoing colonic resection. Based on these results, obesity acts as a negative prognostic factor in the disease process of UC and should enter into discussion that all physicians have with their patients upon initial diagnosis of UC. Studies have found that rates of obesity are increasing amongst the population diagnosed with UC, making this discussion even more crucial to guiding care.
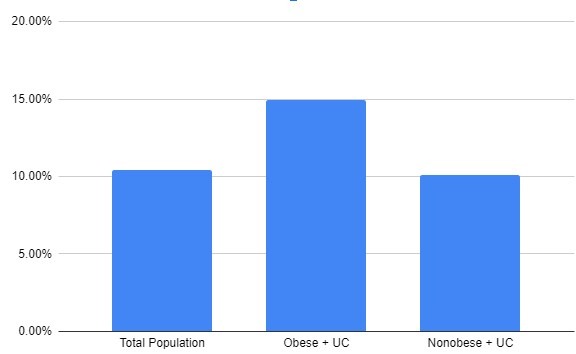
Figure: Figure 1. Graphical representation of nonobese versus obese patients hospitalized for UC who underwent colonic resection during hospitalization. UC = ulcerative colitis
Disclosures:
Laine Lyles indicated no relevant financial relationships.
Eric Klingeman indicated no relevant financial relationships.
James Laney indicated no relevant financial relationships.
Reagan Farmer indicated no relevant financial relationships.
M. Clay O'Brien indicated no relevant financial relationships.
Victoria Sanderford indicated no relevant financial relationships.
William Lyles: ABBVIE Pharmaceuticals – Speakers Bureau.
Laine A. Lyles, DO1, Eric Klingeman, DO2, James Laney, 3, Reagan Farmer, 3, M. Clay O'Brien, BS3, Victoria Sanderford, 4, William E. Lyles, MD, FACG5. A0332 - Obesity as a Prognostic Factor for Colonic Resection in Patients With Ulcerative Colitis: Insights From the National Inpatient Sample, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
