Back

Poster Session B - Monday Morning
Category: Biliary/Pancreas
B0052 - A Case of Severe Acute Alcoholic Pancreatitis Complicated With Abdominal Compartment Syndrome
Monday, October 24, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom
Has Audio

Christopher O. Alabi, MD
HCA East Florida GME Westside/Northwest Internal Medicine
Plantation, FL
Presenting Author(s)
Christopher O. Alabi, MD1, Amaka Onyiagu, MD1, Kelechi Ibe-Ekeocha, MD1, John Romano, MD2, Mayuri Gupta, MD3
1HCA East Florida GME Westside/Northwest Internal Medicine, Plantation, FL; 2HCA Northwest Hospital, Margate, FL; 3HCA Florida Northwest Hospital, Margate, FL
Introduction: Abdominal compartment syndrome (ACS) is a sustained intra-abdominal pressure (IAP) above 20mmHg with associated new-onset organ dysfunction. Even though it is rarely seen in clinical practice, up to 15% of patients with severe acute pancreatitis (SAP) develop ACS and have a mortality rate of up to 49%. Given that delayed treatment of ACS is associated with high mortality and adverse outcome, a higher clinical suspicion is needed to aid diagnosis. We present a case of severe pancreatitis complicated with ACS.
Case Description/Methods: A 29-year-old man with a history of alcohol abuse presented with five days of severe abdominal pain. He was diagnosed with SAP. About 8 hours into admission to the ICU and resuscitation, he began having worsening work of breathing and persistent severe abdominal pain despite being on adequate opioid analgesic. Physical examination revealed tachycardia, diffuse peritoneal signs, guarding, and shock.
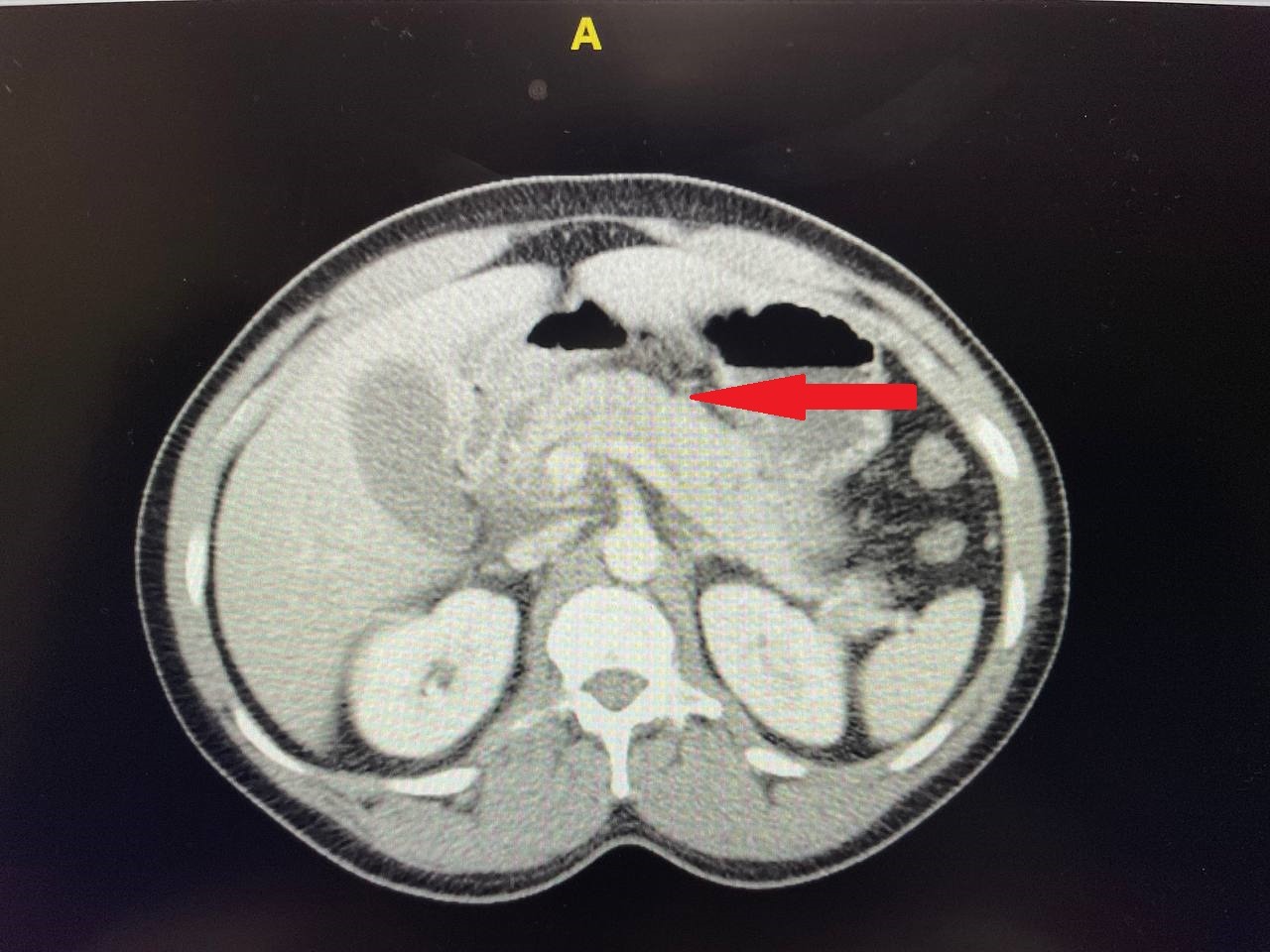
Repeat labs revealed worsening leukocytosis, thrombocytopenia, hyperkalemia, hypocalcemia, lactic acidosis, and elevated creatinine kinase. There was also evidence of renal failure. An edematous pancreas with some peripancreatic fluid collection was evident on the CT abdomen. The abdominal x-ray was unremarkable. Indirect intra-abdominal pressure (IAP) by intravesical catheter pressure measurement was 35mmHg.
He commenced medical management with neuromuscular paralysis and mechanical ventilatory support. A repeat IAP was 24mmHg. He then got surgical decompression by full-thickness midline laparotomy with wound vac placement which further reduced the IAP to 10mmHg. He received serial dialysis, correction of abnormal electrolytes, and serial transfusion with blood products as required. He remained critically ill on a mechanical ventilator and vasopressors, with a poor prognosis at the time of this writing.
Discussion: The pathophysiology of elevated IAP in SAP is multifactorial. These include retroperitoneal inflammation, ascites, acute peripancreatic fluid collections, visceral edema, and aggressive fluid resuscitation. We believe some of the above listed had ensued in our patient for days before he presented to the hospital. Physical examination is inaccurate in diagnosing ACS. The first-line treatment is medical paralysis followed by surgical decompression if ineffective. We are writing this case to recommend early serial IAP measurements in patients with SAP.
Disclosures:
Christopher O. Alabi, MD1, Amaka Onyiagu, MD1, Kelechi Ibe-Ekeocha, MD1, John Romano, MD2, Mayuri Gupta, MD3. B0052 - A Case of Severe Acute Alcoholic Pancreatitis Complicated With Abdominal Compartment Syndrome, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1HCA East Florida GME Westside/Northwest Internal Medicine, Plantation, FL; 2HCA Northwest Hospital, Margate, FL; 3HCA Florida Northwest Hospital, Margate, FL
Introduction: Abdominal compartment syndrome (ACS) is a sustained intra-abdominal pressure (IAP) above 20mmHg with associated new-onset organ dysfunction. Even though it is rarely seen in clinical practice, up to 15% of patients with severe acute pancreatitis (SAP) develop ACS and have a mortality rate of up to 49%. Given that delayed treatment of ACS is associated with high mortality and adverse outcome, a higher clinical suspicion is needed to aid diagnosis. We present a case of severe pancreatitis complicated with ACS.
Case Description/Methods: A 29-year-old man with a history of alcohol abuse presented with five days of severe abdominal pain. He was diagnosed with SAP. About 8 hours into admission to the ICU and resuscitation, he began having worsening work of breathing and persistent severe abdominal pain despite being on adequate opioid analgesic. Physical examination revealed tachycardia, diffuse peritoneal signs, guarding, and shock.
Repeat labs revealed worsening leukocytosis, thrombocytopenia, hyperkalemia, hypocalcemia, lactic acidosis, and elevated creatinine kinase. There was also evidence of renal failure. An edematous pancreas with some peripancreatic fluid collection was evident on the CT abdomen. The abdominal x-ray was unremarkable. Indirect intra-abdominal pressure (IAP) by intravesical catheter pressure measurement was 35mmHg.
He commenced medical management with neuromuscular paralysis and mechanical ventilatory support. A repeat IAP was 24mmHg. He then got surgical decompression by full-thickness midline laparotomy with wound vac placement which further reduced the IAP to 10mmHg. He received serial dialysis, correction of abnormal electrolytes, and serial transfusion with blood products as required. He remained critically ill on a mechanical ventilator and vasopressors, with a poor prognosis at the time of this writing.
Discussion: The pathophysiology of elevated IAP in SAP is multifactorial. These include retroperitoneal inflammation, ascites, acute peripancreatic fluid collections, visceral edema, and aggressive fluid resuscitation. We believe some of the above listed had ensued in our patient for days before he presented to the hospital. Physical examination is inaccurate in diagnosing ACS. The first-line treatment is medical paralysis followed by surgical decompression if ineffective. We are writing this case to recommend early serial IAP measurements in patients with SAP.
Figure: CT abdomen showing edematous pancreas with some peripancreatic fluid collection
Disclosures:
Christopher Alabi indicated no relevant financial relationships.
Amaka Onyiagu indicated no relevant financial relationships.
Kelechi Ibe-Ekeocha indicated no relevant financial relationships.
John Romano indicated no relevant financial relationships.
Mayuri Gupta indicated no relevant financial relationships.
Christopher O. Alabi, MD1, Amaka Onyiagu, MD1, Kelechi Ibe-Ekeocha, MD1, John Romano, MD2, Mayuri Gupta, MD3. B0052 - A Case of Severe Acute Alcoholic Pancreatitis Complicated With Abdominal Compartment Syndrome, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.

