Back

Poster Session B - Monday Morning
Category: Interventional Endoscopy
B0464 - Malnutrition and Post-ERCP Complications: Nationwide Inpatient Sample Database Analysis
Monday, October 24, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom
Has Audio

Anjella Manoharan, MS, MD
Rutgers New Jersey Medical School
Newark, NJ
Presenting Author(s)
Anjella Manoharan, MS, MD, Vincent Wong, MD, Dayna Panchal, DO, Weizheng Wang, MD
Rutgers New Jersey Medical School, Newark, NJ
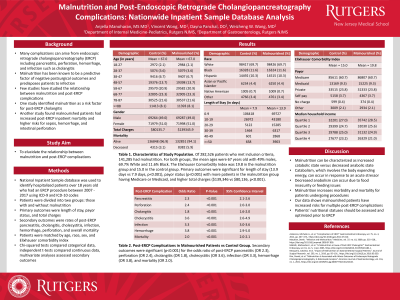
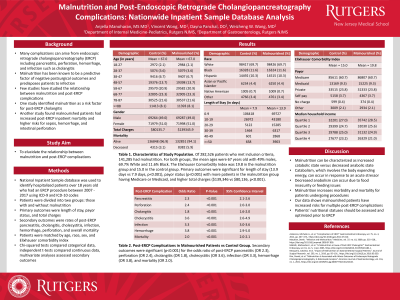
Introduction: Complications can arise from endoscopic retrograde cholangiopancreatography (ERCP). Few studies have studied the relationship between malnutrition and post-ERCP complications. One study identified malnutrition as a risk factor for post-ERCP cholangitis. Another study found malnourished patients had increased post-ERCP inpatient mortality and higher risks for sepsis, hemorrhage, and intestinal perforation. We seek to elucidate the relationship between malnutrition and post-ERCP complications.
Methods: The National Inpatient Sample database was used to identify hospitalized patients over 18 years old who had an ERCP procedure between 2007 - 2017 using ICD-9 and ICD-10 codes. Patients were divided into two groups, those with and without malnutrition. Primary outcomes were length of stay, payor status, and total charges. Secondary outcomes were rates of post-ERCP pancreatitis, cholangitis, cholecystitis, infection, hemorrhage, perforation, and overall mortality. Patients were matched by age, race, sex, and Elixhauser comorbidity index. Chi-squared tests compared categorical data, independent t-tests compared continuous data, and multivariate analyses assessed primary outcomes.
Results: Of 282,526 patients who met inclusion criteria, 141,285 had malnutrition. For both groups, the mean ages were 67 years old with 49% males, 69.7% White and 11.6% Black. The Elixhauser Comorbidity Index was 19.8 in the malnutrition group and 15.0 in the control group. Primary outcomes were significant for length of stay (13.9 days vs 7.9 days, p< 0.001), payor status (p< 0.001) with more patients in the malnutrition group having Medicare or Medicaid, and higher total charges ($139,346 vs $80,136, p< 0.001). Secondary outcomes were significant (p< 0.001) for the odds ratio of post-ERCP pancreatitis (OR 2.3), perforation (OR 2.4), cholangitis (OR 1.8), cholecystitis (OR 3.6), infection (OR 3.3), hemorrhage (OR 3.8), and mortality (OR 2.0).
Discussion: Malnutrition can be characterized as increased catabolic state versus decreased anabolic state. Catabolism, which involves the body expending energy, can occur in response to an acute stressor. Decreased anabolism can occur due to food insecurity or feeding issues. Malnutrition increases morbidity and mortality for patients undergoing procedures. Our data shows malnourished patients have increased risks for multiple post-ERCP complications. Patients’ nutritional statuses should be assessed and optimized prior to ERCP.
Disclosures:
Anjella Manoharan, MS, MD, Vincent Wong, MD, Dayna Panchal, DO, Weizheng Wang, MD. B0464 - Malnutrition and Post-ERCP Complications: Nationwide Inpatient Sample Database Analysis, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
Rutgers New Jersey Medical School, Newark, NJ
Introduction: Complications can arise from endoscopic retrograde cholangiopancreatography (ERCP). Few studies have studied the relationship between malnutrition and post-ERCP complications. One study identified malnutrition as a risk factor for post-ERCP cholangitis. Another study found malnourished patients had increased post-ERCP inpatient mortality and higher risks for sepsis, hemorrhage, and intestinal perforation. We seek to elucidate the relationship between malnutrition and post-ERCP complications.
Methods: The National Inpatient Sample database was used to identify hospitalized patients over 18 years old who had an ERCP procedure between 2007 - 2017 using ICD-9 and ICD-10 codes. Patients were divided into two groups, those with and without malnutrition. Primary outcomes were length of stay, payor status, and total charges. Secondary outcomes were rates of post-ERCP pancreatitis, cholangitis, cholecystitis, infection, hemorrhage, perforation, and overall mortality. Patients were matched by age, race, sex, and Elixhauser comorbidity index. Chi-squared tests compared categorical data, independent t-tests compared continuous data, and multivariate analyses assessed primary outcomes.
Results: Of 282,526 patients who met inclusion criteria, 141,285 had malnutrition. For both groups, the mean ages were 67 years old with 49% males, 69.7% White and 11.6% Black. The Elixhauser Comorbidity Index was 19.8 in the malnutrition group and 15.0 in the control group. Primary outcomes were significant for length of stay (13.9 days vs 7.9 days, p< 0.001), payor status (p< 0.001) with more patients in the malnutrition group having Medicare or Medicaid, and higher total charges ($139,346 vs $80,136, p< 0.001). Secondary outcomes were significant (p< 0.001) for the odds ratio of post-ERCP pancreatitis (OR 2.3), perforation (OR 2.4), cholangitis (OR 1.8), cholecystitis (OR 3.6), infection (OR 3.3), hemorrhage (OR 3.8), and mortality (OR 2.0).
Discussion: Malnutrition can be characterized as increased catabolic state versus decreased anabolic state. Catabolism, which involves the body expending energy, can occur in response to an acute stressor. Decreased anabolism can occur due to food insecurity or feeding issues. Malnutrition increases morbidity and mortality for patients undergoing procedures. Our data shows malnourished patients have increased risks for multiple post-ERCP complications. Patients’ nutritional statuses should be assessed and optimized prior to ERCP.
Disclosures:
Anjella Manoharan indicated no relevant financial relationships.
Vincent Wong indicated no relevant financial relationships.
Dayna Panchal indicated no relevant financial relationships.
Weizheng Wang indicated no relevant financial relationships.
Anjella Manoharan, MS, MD, Vincent Wong, MD, Dayna Panchal, DO, Weizheng Wang, MD. B0464 - Malnutrition and Post-ERCP Complications: Nationwide Inpatient Sample Database Analysis, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
