Back

Poster Session A - Sunday Afternoon
Category: Stomach
A0712 - Vagal Nerve Injury Presenting as Acute Gastric Outlet Obstruction: A Rare Case Presentation
Sunday, October 23, 2022
5:00 PM – 7:00 PM ET
Location: Crown Ballroom
Has Audio

Harsh Jain, DO
Montefiore Medical Center
Jersey City, NJ
Presenting Author(s)
Harsh Jain, DO1, Nicholas Costable, MD2, Harish Guddati, MD, 2
1Montefiore Medical Center, Jersey City, NJ; 2Montefiore Medical Center, Bronx, NY
Introduction: Gastroparesis is a syndrome of delayed gastric emptying in the absence of a mechanical obstruction. While the majority of cases of gastroparesis are idiopathic or related to poorly controlled diabetes (DM), it may also arise as a complication of surgery or from vagal nerve injury. Procedures including carotid endarterectomy, anti-reflux surgery, aortic aneurysm repair, and heart and lung transplants have been reported to cause vagal nerve injury. We report the rare case of a patient experiencing an inadvertent vagal nerve injury leading to gastroparesis and subsequent gastric outlet obstruction (GOO).
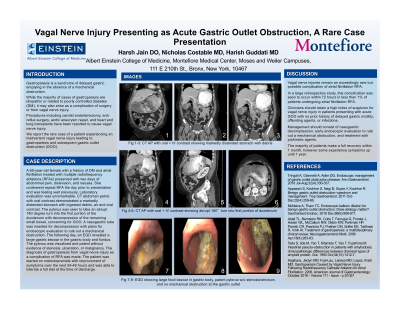
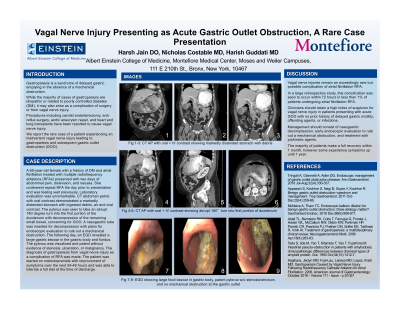
Case Description/Methods: A 60-year-old female with a history of DM and atrial fibrillation treated with multiple radiofrequency ablations (RFAs) presented with two days of abdominal pain, distension, and nausea. She underwent repeat RFA the day prior to presentation and was feeling well previously. Laboratory evaluation was unremarkable. CT abdomen pelvis with oral contrast demonstrated a markedly distended stomach with ingested debris, air and oral contrast. The pylorus was seen to take an abrupt 180 degree turn into the first portion of the duodenum with decompression of the remaining small bowel, concerning for GOO. A nasogastric tube was inserted for decompression with plans for endoscopic evaluation to rule out a mechanical obstruction. The following day, an EGD revealed a large gastric bezoar in the gastric body and fundus. The pylorus was visualized and patent without evidence of stenosis, ulceration, or malignancy. The diagnosis of gastroparesis from vagal nerve injury as a complication of RFA was made. The patient was started on metoclopramide with improvement of symptoms over the next 24-48 hours and was able to tolerate a full diet at the time of discharge.
Discussion: Vagal nerve injuries remain an exceedingly rare but possible complication of atrial fibrillation RFA. In a large retrospective study, this complication was seen to occur within 72 hours in less than 1% of patients undergoing atrial fibrillation RFA. Clinicians should retain a high index of suspicion for vagal nerve injury in patients presenting with acute GOO with no prior history of delayed gastric motility, offending agents, or infections. Management should consist of nasogastric decompression, early endoscopic evaluation to rule out a mechanical obstruction, and treatment with prokinetic agents. The majority of patients make a full recovery within 1 month, however some experience symptoms up until 1 year.
Disclosures:
Harsh Jain, DO1, Nicholas Costable, MD2, Harish Guddati, MD, 2. A0712 - Vagal Nerve Injury Presenting as Acute Gastric Outlet Obstruction: A Rare Case Presentation, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1Montefiore Medical Center, Jersey City, NJ; 2Montefiore Medical Center, Bronx, NY
Introduction: Gastroparesis is a syndrome of delayed gastric emptying in the absence of a mechanical obstruction. While the majority of cases of gastroparesis are idiopathic or related to poorly controlled diabetes (DM), it may also arise as a complication of surgery or from vagal nerve injury. Procedures including carotid endarterectomy, anti-reflux surgery, aortic aneurysm repair, and heart and lung transplants have been reported to cause vagal nerve injury. We report the rare case of a patient experiencing an inadvertent vagal nerve injury leading to gastroparesis and subsequent gastric outlet obstruction (GOO).
Case Description/Methods: A 60-year-old female with a history of DM and atrial fibrillation treated with multiple radiofrequency ablations (RFAs) presented with two days of abdominal pain, distension, and nausea. She underwent repeat RFA the day prior to presentation and was feeling well previously. Laboratory evaluation was unremarkable. CT abdomen pelvis with oral contrast demonstrated a markedly distended stomach with ingested debris, air and oral contrast. The pylorus was seen to take an abrupt 180 degree turn into the first portion of the duodenum with decompression of the remaining small bowel, concerning for GOO. A nasogastric tube was inserted for decompression with plans for endoscopic evaluation to rule out a mechanical obstruction. The following day, an EGD revealed a large gastric bezoar in the gastric body and fundus. The pylorus was visualized and patent without evidence of stenosis, ulceration, or malignancy. The diagnosis of gastroparesis from vagal nerve injury as a complication of RFA was made. The patient was started on metoclopramide with improvement of symptoms over the next 24-48 hours and was able to tolerate a full diet at the time of discharge.
Discussion: Vagal nerve injuries remain an exceedingly rare but possible complication of atrial fibrillation RFA. In a large retrospective study, this complication was seen to occur within 72 hours in less than 1% of patients undergoing atrial fibrillation RFA. Clinicians should retain a high index of suspicion for vagal nerve injury in patients presenting with acute GOO with no prior history of delayed gastric motility, offending agents, or infections. Management should consist of nasogastric decompression, early endoscopic evaluation to rule out a mechanical obstruction, and treatment with prokinetic agents. The majority of patients make a full recovery within 1 month, however some experience symptoms up until 1 year.
Disclosures:
Harsh Jain indicated no relevant financial relationships.
Nicholas Costable indicated no relevant financial relationships.
Harish Guddati, MD indicated no relevant financial relationships.
Harsh Jain, DO1, Nicholas Costable, MD2, Harish Guddati, MD, 2. A0712 - Vagal Nerve Injury Presenting as Acute Gastric Outlet Obstruction: A Rare Case Presentation, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
