Back

Poster Session A - Sunday Afternoon
Category: Liver
A0537 - Severe Noncirrhotic Hyperammonemia: What Urea-lly Should Consider
Sunday, October 23, 2022
5:00 PM – 7:00 PM ET
Location: Crown Ballroom
Has Audio

Samantha Wu, MD
Tulane University School of Medicine
New Orleans, LA
Presenting Author(s)
Samantha Wu, MD, Carlo S. Basilio, MD, MPH
Tulane University School of Medicine, New Orleans, LA
Introduction: Hyperammonemia is often the result of liver pathology. When hyperammonemia is not the result of liver disease, an occult disorder of metabolism must be on the differential for unexplained hyperammonemia, such as a urea cycle disorder (UCD).
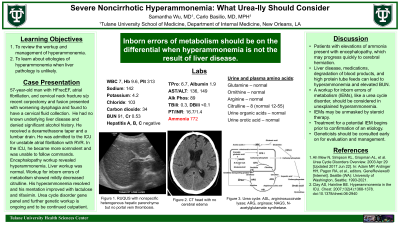
Case Description/Methods: A 57-year-old man with heart failure with recovered ejection fraction, atrial fibrillation, hypertension, and cervical neck fracture who had undergone a recent cervical spine corpectomy and fusion presented with worsening dysphagia and was found to have a cervical fluid collection for which he received a dexamethasone taper and a lumbar drain. He had no known underlying liver disease and denied significant alcohol history. He was later admitted to the intensive care unit (ICU) for unstable atrial fibrillation with rapid ventricular response (RVR). In the ICU, he became more somnolent and was unable to follow commands. Encephalopathy workup was significant for elevated BUN with normal creatinine, ammonia 772, and mildly elevated transaminases. His labs and imaging did not demonstrate cirrhosis or acute liver failure. Workup for inborn errors of metabolism showed mildly decreased citrulline. Urine and plasma amino acids were otherwise normal. His hyperammonemia resolved and his mentation improved with lactulose and rifaximin. UCD gene panel and further genetic workup is ongoing and to be continued outpatient.
Discussion: Patients with elevations of ammonia present with encephalopathy, which may progress quickly to cerebral herniation. Survival requires immediate reduction of ammonia levels. Although the differential for hyperammonemia is broad, inborn errors of metabolism (IEM), like a UCD, should be considered when hyperammonemia is of unclear etiology. This patient’s liver workup revealed no findings consistent with cirrhosis or liver failure. Potential causes for his hyperammonemia include ischemic liver disease secondary to atrial fibrillation with RVR or degradation of blood products. IEMs may also be unmasked by steroid therapy, which is plausible in this patient who was on a steroid taper prior to his hyperammonemic state. Although IEMs often have early age of onset, UCDs have multiple modes of inheritance and can present at later stage. Ornithine transcarbamylase deficiency is the most common UCD and can present with reduced plasma citrulline in both kids and adults. Treatment for a potential IEM begins prior to confirmation of an etiology. Geneticists should be consulted early on for evaluation and management.
Disclosures:
Samantha Wu, MD, Carlo S. Basilio, MD, MPH. A0537 - Severe Noncirrhotic Hyperammonemia: What Urea-lly Should Consider, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
Tulane University School of Medicine, New Orleans, LA
Introduction: Hyperammonemia is often the result of liver pathology. When hyperammonemia is not the result of liver disease, an occult disorder of metabolism must be on the differential for unexplained hyperammonemia, such as a urea cycle disorder (UCD).
Case Description/Methods: A 57-year-old man with heart failure with recovered ejection fraction, atrial fibrillation, hypertension, and cervical neck fracture who had undergone a recent cervical spine corpectomy and fusion presented with worsening dysphagia and was found to have a cervical fluid collection for which he received a dexamethasone taper and a lumbar drain. He had no known underlying liver disease and denied significant alcohol history. He was later admitted to the intensive care unit (ICU) for unstable atrial fibrillation with rapid ventricular response (RVR). In the ICU, he became more somnolent and was unable to follow commands. Encephalopathy workup was significant for elevated BUN with normal creatinine, ammonia 772, and mildly elevated transaminases. His labs and imaging did not demonstrate cirrhosis or acute liver failure. Workup for inborn errors of metabolism showed mildly decreased citrulline. Urine and plasma amino acids were otherwise normal. His hyperammonemia resolved and his mentation improved with lactulose and rifaximin. UCD gene panel and further genetic workup is ongoing and to be continued outpatient.
Discussion: Patients with elevations of ammonia present with encephalopathy, which may progress quickly to cerebral herniation. Survival requires immediate reduction of ammonia levels. Although the differential for hyperammonemia is broad, inborn errors of metabolism (IEM), like a UCD, should be considered when hyperammonemia is of unclear etiology. This patient’s liver workup revealed no findings consistent with cirrhosis or liver failure. Potential causes for his hyperammonemia include ischemic liver disease secondary to atrial fibrillation with RVR or degradation of blood products. IEMs may also be unmasked by steroid therapy, which is plausible in this patient who was on a steroid taper prior to his hyperammonemic state. Although IEMs often have early age of onset, UCDs have multiple modes of inheritance and can present at later stage. Ornithine transcarbamylase deficiency is the most common UCD and can present with reduced plasma citrulline in both kids and adults. Treatment for a potential IEM begins prior to confirmation of an etiology. Geneticists should be consulted early on for evaluation and management.
Disclosures:
Samantha Wu indicated no relevant financial relationships.
Carlo Basilio indicated no relevant financial relationships.
Samantha Wu, MD, Carlo S. Basilio, MD, MPH. A0537 - Severe Noncirrhotic Hyperammonemia: What Urea-lly Should Consider, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.

