Back
Poster Session B - Monday Morning
Category: IBD
B0372 - Endoscopic Disease Activity and Biologic Therapy Are Independent Predictors of Suboptimal Bowel Preparation in Patients With Inflammatory Bowel Disease Undergoing Colonoscopy: A Multicenter Analysis
Monday, October 24, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom
.jpg)
Anand Kumar, MD
Lenox Hill Hospital
New York, New York
Presenting Author(s)
Award: Presidential Poster Award
Anand Kumar, MD1, Emily Bae, 2, Ellen Osemi, MD3, Ogooluwa Fayemiwo, MPH1, Vinayak Shenoy, DO1, Priyanka Singh, MD3, Megan C. Buckley, DO4, Laura Durbin, MPH1, James Mackey, MPH1, Dana Lukin, MD, PhD5, Keith Sultan, MD6, Arun Swaminath, MD7
1Lenox Hill Hospital, New York, NY; 2Weill Cornell Medical College, New York, NY; 3Long Island Jewish Medical Center, Queens, NY; 4Northwell Health, Lenox Hill Hospital, New York, NY; 5Weill Cornell Medicine, New York, NY; 6Long Island Jewish Medical Center, North Shore University Hospital, Long Island, NY; 7Northwell Health, Lenox Hill Hospital, Manhattan, NY
Introduction: Optimal bowel preparation (BP) is critical for endoscopic assessment of inflammation and dysplasia in patients with inflammatory bowel disease (IBD). Comorbidities and patient-related factors have been associated with sub-optimal BP (SOBP) in the general population. Using a multicenter database, we sought to identify disease-specific characteristics that may impact the quality of BP in patients with IBD.
Methods: We conducted a retrospective analysis of adult IBD patients who underwent outpatient colonoscopies between January 2011 and October 2021 at three large academic medical centers. Patients with total colectomy or those undergoing only sigmoidoscopy were excluded. Quality of BP was documented using the Boston Bowel Preparation Scale (BBPS) or the Aronchick scale and dichotomized into “sub-optimal” (BBPS 0-5 or Aronchick “fair”, “poor”, unsatisfactory”) and “optimal” (BBPS 6-9 or Aronchick “excellent”, “good”). The primary objective was to evaluate IBD-specific factors associated with SOBP. Independent associations were calculated using multivariable backward stepwise regression models.
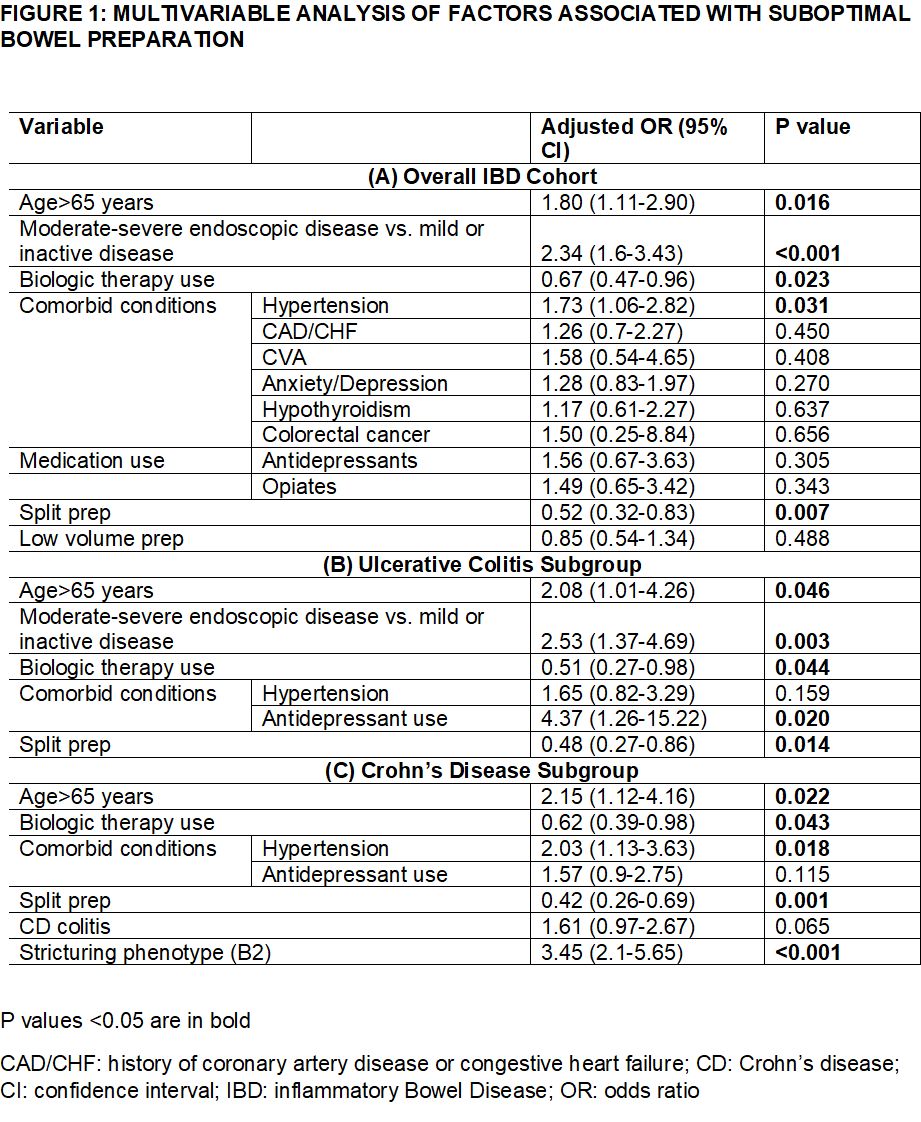
Results: Among a total of 1154 IBD patients [53% females, mean age 47±17 years, 58% with Crohn’s disease (CD), 40% with ulcerative colitis (UC), 23% with moderate-to-severe disease, 40% receiving biologic therapy], 23.5% (N=271) had SOBP. 69% of patients received a low-volume prep (≤2L) and 80% received it in a split-dose format. Cecal or anastomotic intubation was achieved in 94% of patients. On multivariable analysis, moderate-to-severe endoscopic disease versus mild or inactive disease was associated with a higher odds of SOBP [OR 2.34 (1.60-3.43)] whereas baseline biologic use was associated with a lower odds of SOBP [OR 0.67 (0.47-0.96)] among the overall IBD cohort. Additionally, age >65 years [OR 1.80 (1.11-2.90)] and hypertension [OR 1.73 (1.06-2.82)] predicted higher odds, and split-dose (vs single-dose) BP [OR 0.52 (0.32-0.83)] predicted a lower odds of SOBP among IBD patients (Fig 1-A). In the subgroup analysis, biologic therapy use, age >65 years, and split-dose BP were predictors of SOBP in both UC and CD subgroups, whereas stricturing phenotype predicted SOBP among the CD cohort (Fig 1- B,C).
Discussion: Endoscopic disease activity was predictive of SOBP, and biologic therapy was protective against SOBP among IBD patients. Improved inflammatory control using biologic therapies may also improve quality of BP among IBD patients undergoing colonoscopy.
Disclosures:
Anand Kumar, MD1, Emily Bae, 2, Ellen Osemi, MD3, Ogooluwa Fayemiwo, MPH1, Vinayak Shenoy, DO1, Priyanka Singh, MD3, Megan C. Buckley, DO4, Laura Durbin, MPH1, James Mackey, MPH1, Dana Lukin, MD, PhD5, Keith Sultan, MD6, Arun Swaminath, MD7. B0372 - Endoscopic Disease Activity and Biologic Therapy Are Independent Predictors of Suboptimal Bowel Preparation in Patients With Inflammatory Bowel Disease Undergoing Colonoscopy: A Multicenter Analysis, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
Anand Kumar, MD1, Emily Bae, 2, Ellen Osemi, MD3, Ogooluwa Fayemiwo, MPH1, Vinayak Shenoy, DO1, Priyanka Singh, MD3, Megan C. Buckley, DO4, Laura Durbin, MPH1, James Mackey, MPH1, Dana Lukin, MD, PhD5, Keith Sultan, MD6, Arun Swaminath, MD7
1Lenox Hill Hospital, New York, NY; 2Weill Cornell Medical College, New York, NY; 3Long Island Jewish Medical Center, Queens, NY; 4Northwell Health, Lenox Hill Hospital, New York, NY; 5Weill Cornell Medicine, New York, NY; 6Long Island Jewish Medical Center, North Shore University Hospital, Long Island, NY; 7Northwell Health, Lenox Hill Hospital, Manhattan, NY
Introduction: Optimal bowel preparation (BP) is critical for endoscopic assessment of inflammation and dysplasia in patients with inflammatory bowel disease (IBD). Comorbidities and patient-related factors have been associated with sub-optimal BP (SOBP) in the general population. Using a multicenter database, we sought to identify disease-specific characteristics that may impact the quality of BP in patients with IBD.
Methods: We conducted a retrospective analysis of adult IBD patients who underwent outpatient colonoscopies between January 2011 and October 2021 at three large academic medical centers. Patients with total colectomy or those undergoing only sigmoidoscopy were excluded. Quality of BP was documented using the Boston Bowel Preparation Scale (BBPS) or the Aronchick scale and dichotomized into “sub-optimal” (BBPS 0-5 or Aronchick “fair”, “poor”, unsatisfactory”) and “optimal” (BBPS 6-9 or Aronchick “excellent”, “good”). The primary objective was to evaluate IBD-specific factors associated with SOBP. Independent associations were calculated using multivariable backward stepwise regression models.
Results: Among a total of 1154 IBD patients [53% females, mean age 47±17 years, 58% with Crohn’s disease (CD), 40% with ulcerative colitis (UC), 23% with moderate-to-severe disease, 40% receiving biologic therapy], 23.5% (N=271) had SOBP. 69% of patients received a low-volume prep (≤2L) and 80% received it in a split-dose format. Cecal or anastomotic intubation was achieved in 94% of patients. On multivariable analysis, moderate-to-severe endoscopic disease versus mild or inactive disease was associated with a higher odds of SOBP [OR 2.34 (1.60-3.43)] whereas baseline biologic use was associated with a lower odds of SOBP [OR 0.67 (0.47-0.96)] among the overall IBD cohort. Additionally, age >65 years [OR 1.80 (1.11-2.90)] and hypertension [OR 1.73 (1.06-2.82)] predicted higher odds, and split-dose (vs single-dose) BP [OR 0.52 (0.32-0.83)] predicted a lower odds of SOBP among IBD patients (Fig 1-A). In the subgroup analysis, biologic therapy use, age >65 years, and split-dose BP were predictors of SOBP in both UC and CD subgroups, whereas stricturing phenotype predicted SOBP among the CD cohort (Fig 1- B,C).
Discussion: Endoscopic disease activity was predictive of SOBP, and biologic therapy was protective against SOBP among IBD patients. Improved inflammatory control using biologic therapies may also improve quality of BP among IBD patients undergoing colonoscopy.
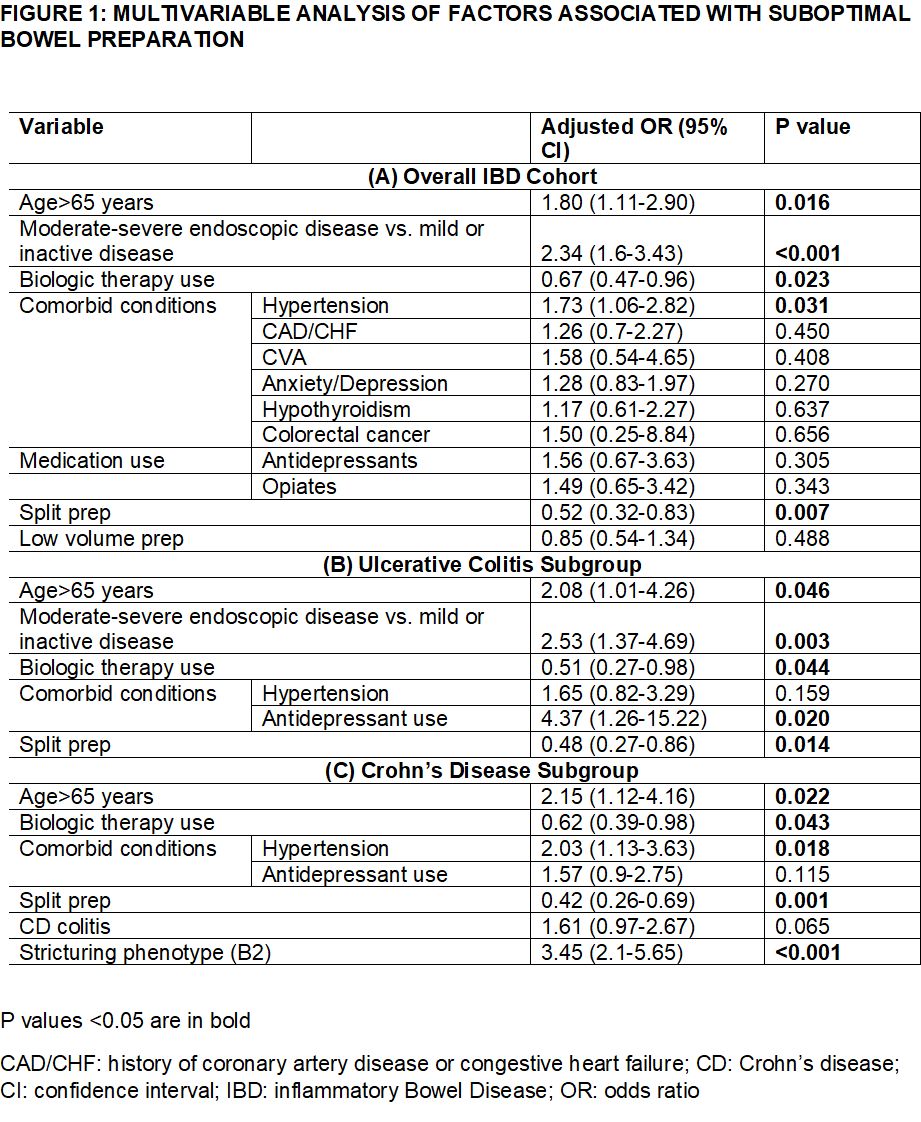
Figure: Figure 1 (A, B, C): Multivariable analysis of factors associated with suboptimal bowel preparation in patients with IBD
Disclosures:
Anand Kumar indicated no relevant financial relationships.
Emily Bae indicated no relevant financial relationships.
Ellen Osemi indicated no relevant financial relationships.
Ogooluwa Fayemiwo indicated no relevant financial relationships.
Vinayak Shenoy indicated no relevant financial relationships.
Priyanka Singh indicated no relevant financial relationships.
Megan Buckley indicated no relevant financial relationships.
Laura Durbin indicated no relevant financial relationships.
James Mackey indicated no relevant financial relationships.
Dana Lukin: AbbVie – Consultant, Grant/Research Support. Boehringer Ingelheim – Consultant. Bristol Myers Squibb – Consultant. Eli Lilly – Consultant. Janssen – Consultant, Grant/Research Support. Palatin Technologies – Consultant. Pfizer – Consultant. Takeda – Grant/Research Support.
Keith Sultan indicated no relevant financial relationships.
Arun Swaminath: BI – Advisory Committee/Board Member. BMS – Advisory Committee/Board Member. Janssen – Grant/Research Support. Takeda – Grant/Research Support.
Anand Kumar, MD1, Emily Bae, 2, Ellen Osemi, MD3, Ogooluwa Fayemiwo, MPH1, Vinayak Shenoy, DO1, Priyanka Singh, MD3, Megan C. Buckley, DO4, Laura Durbin, MPH1, James Mackey, MPH1, Dana Lukin, MD, PhD5, Keith Sultan, MD6, Arun Swaminath, MD7. B0372 - Endoscopic Disease Activity and Biologic Therapy Are Independent Predictors of Suboptimal Bowel Preparation in Patients With Inflammatory Bowel Disease Undergoing Colonoscopy: A Multicenter Analysis, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.


