Back

Poster Session A - Sunday Afternoon
Category: Liver
A0573 - Primary Hepatic Diffuse Large B Cell Lymphoma Presenting as a Picture of Acute Alcoholic Hepatitis
Sunday, October 23, 2022
5:00 PM – 7:00 PM ET
Location: Crown Ballroom
Has Audio
- SC
Sreenidhi Chintalapani, MD
HCA Healthcare Eastern Idaho Regional Medical Center
Idaho Falls, ID
Presenting Author(s)
Sreenidhi Chintalapani, MD1, Bryce Chavez, MD1, John H. Grider, DO2
1HCA Healthcare Eastern Idaho Regional Medical Center, Idaho Falls, ID; 2Eastern Idaho Regional Medical Center, Idaho Falls, ID
Introduction: Diffuse large B cell lymphoma (DLBCL) is a prevalent subcategory of Non-Hodgkin lymphoma (NHL) comprising around 25% of all NHL occurrences. Generally, 60% of cases will present with Stage III/IV advanced disease vs 40% with localized disease. While DLBCL can arise from any tissue, 40% of cases will come from extranodal extramedullary tissue; most commonly the stomach or GI. Interestingly, primary hepatic lymphoma is exceedingly rare with a reported incidence of 0.4% of all extranodal NHL and 0.016% for all NHL. The presentation can be vague and a mimicker of other disease with symptoms such as abdominal pain, bloating, nausea, vomiting, and B symptoms.
Case Description/Methods: A 59-year-old female with no significant medical history presented for dizziness, fatigue, fever, shortness of breath, weight loss, night sweats, chills x1 month. She drinks 18 beers/week and is employed at a bar. Initially found to have thrombocytopenia, transaminitis (AST >ALT), hepatosplenomegaly, hypotension, normocytic anemia, latent hepatitis B, and a pulmonary embolism. Her hepatitis was thought to be secondary to alcoholic hepatitis. Her MELD was 12 and Maddrey of -0.6. GI was consulted, further workup showed a past EBV and CMV infection. Quantiferon, HIV, mono, autoimmune and rheumatologic workup were negative. Ultimately a liver biopsy was positive for DLBCL. She was vaccinated for encapsulated organisms, treated for her Hepatitis B, and initiated on R-EPOCH regimen. She was transitioned to RCHOP and ultimately had no evidence of FDG presence on PET Scan and complete response to therapy. She was advised to have routine surveillance per NCCN guidelines.
Discussion: Primary hepatic DLBCL is rare and not often diagnosed when a patient presents with acute hepatitis and known risk factors of alcohol use. However, our patient had multiple B-symptoms concerning for lymphoma. The only way to definitively diagnose DLBCL is by liver biopsy with the prevailing management of EPOCH chemotherapy. Early diagnosis and initiation of treatment is crucial due to its poor prognosis and advanced stage presentation. For this reason, a broad differential diagnosis must be considered when evaluating patients with alcoholic hepatitis.
This research was supported (in whole or in part) by HCA Healthcare and/or an HCA Healthcare affiliated entity. The views expressed in this publication represent those of the author(s) and do not necessarily represent the official views of HCA Healthcare or any of its affiliated entities.
Disclosures:
Sreenidhi Chintalapani, MD1, Bryce Chavez, MD1, John H. Grider, DO2. A0573 - Primary Hepatic Diffuse Large B Cell Lymphoma Presenting as a Picture of Acute Alcoholic Hepatitis, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1HCA Healthcare Eastern Idaho Regional Medical Center, Idaho Falls, ID; 2Eastern Idaho Regional Medical Center, Idaho Falls, ID
Introduction: Diffuse large B cell lymphoma (DLBCL) is a prevalent subcategory of Non-Hodgkin lymphoma (NHL) comprising around 25% of all NHL occurrences. Generally, 60% of cases will present with Stage III/IV advanced disease vs 40% with localized disease. While DLBCL can arise from any tissue, 40% of cases will come from extranodal extramedullary tissue; most commonly the stomach or GI. Interestingly, primary hepatic lymphoma is exceedingly rare with a reported incidence of 0.4% of all extranodal NHL and 0.016% for all NHL. The presentation can be vague and a mimicker of other disease with symptoms such as abdominal pain, bloating, nausea, vomiting, and B symptoms.
Case Description/Methods: A 59-year-old female with no significant medical history presented for dizziness, fatigue, fever, shortness of breath, weight loss, night sweats, chills x1 month. She drinks 18 beers/week and is employed at a bar. Initially found to have thrombocytopenia, transaminitis (AST >ALT), hepatosplenomegaly, hypotension, normocytic anemia, latent hepatitis B, and a pulmonary embolism. Her hepatitis was thought to be secondary to alcoholic hepatitis. Her MELD was 12 and Maddrey of -0.6. GI was consulted, further workup showed a past EBV and CMV infection. Quantiferon, HIV, mono, autoimmune and rheumatologic workup were negative. Ultimately a liver biopsy was positive for DLBCL. She was vaccinated for encapsulated organisms, treated for her Hepatitis B, and initiated on R-EPOCH regimen. She was transitioned to RCHOP and ultimately had no evidence of FDG presence on PET Scan and complete response to therapy. She was advised to have routine surveillance per NCCN guidelines.
Discussion: Primary hepatic DLBCL is rare and not often diagnosed when a patient presents with acute hepatitis and known risk factors of alcohol use. However, our patient had multiple B-symptoms concerning for lymphoma. The only way to definitively diagnose DLBCL is by liver biopsy with the prevailing management of EPOCH chemotherapy. Early diagnosis and initiation of treatment is crucial due to its poor prognosis and advanced stage presentation. For this reason, a broad differential diagnosis must be considered when evaluating patients with alcoholic hepatitis.
This research was supported (in whole or in part) by HCA Healthcare and/or an HCA Healthcare affiliated entity. The views expressed in this publication represent those of the author(s) and do not necessarily represent the official views of HCA Healthcare or any of its affiliated entities.
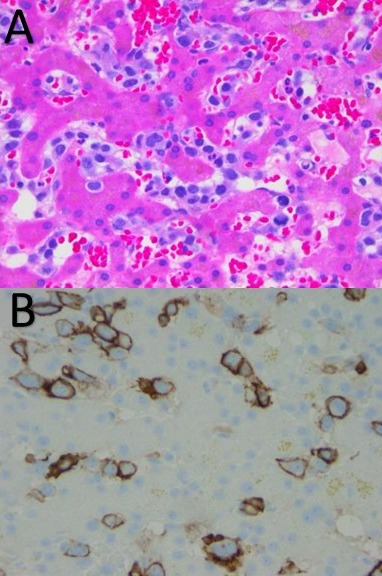
Figure: A: Markedly atypical lymphoid infiltrate involving both the hepatic sinusoids and portal tracts. The lymphocytes are large with vesicular chromatin, prominent nucleoli, and fairly abundant mitotic activity
B: Immunohistochemical stains are performed . The atypical lymphocytes react with CD20, PAX5, and coexpress BCL-2 (90%) and C-MYC (60%).
B: Immunohistochemical stains are performed . The atypical lymphocytes react with CD20, PAX5, and coexpress BCL-2 (90%) and C-MYC (60%).
Disclosures:
Sreenidhi Chintalapani indicated no relevant financial relationships.
Bryce Chavez indicated no relevant financial relationships.
John Grider indicated no relevant financial relationships.
Sreenidhi Chintalapani, MD1, Bryce Chavez, MD1, John H. Grider, DO2. A0573 - Primary Hepatic Diffuse Large B Cell Lymphoma Presenting as a Picture of Acute Alcoholic Hepatitis, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
