Back

Poster Session A - Sunday Afternoon
Category: Liver
A0580 - Hepatitis With an Unknown Etiology with Concomitant ITP
Sunday, October 23, 2022
5:00 PM – 7:00 PM ET
Location: Crown Ballroom
Has Audio

Ariana R. Tagliaferri, MD
Saint Joseph's University Medical Center
Paterson, NJ
Presenting Author(s)
Brooke E. Kania, DO1, Ariana Tagliaferri, MD2, Dhruv Patel, DO2, Iqra Baig, 2, Alisa Farokhian, MD2
1Saint Joseph's University Medical Center, Parsippany-Troy Hills, NJ; 2St. Joseph's University Medical Center, Paterson, NJ
Introduction: Alcoholic hepatitis (AH) usually presents after decades of alcohol consumption and can even manifest with recent abstinence. The clinical presentation may be compounded by underlying liver cirrhosis and LFT’s are not a reliable means of diagnosing AH due to poor sensitivity and specificity. Hepatitis is only one of the major causes of thrombocytopenia. Immune thrombocytopenic purpura (ITP) is a diagnosis of exclusion and further workup is warranted with persistent thrombocytopenia refractory to treatment for AH. Although there is limited data demonstrating a correlation between AH and ITP, both conditions respond to steroids. We present a case of a 42 YO M with an unknown cause of hepatitis and concomitant ITP who responded well to steroids.
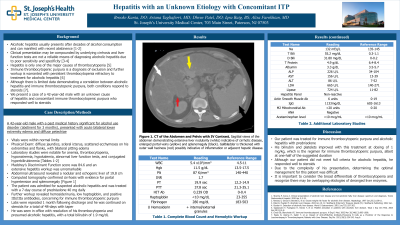
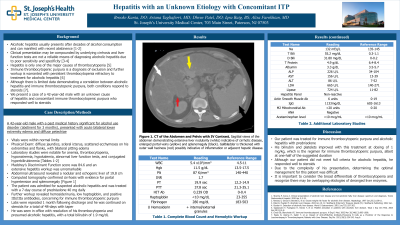
Case Description/Methods: A 42 YO M PMH of alcohol use disorder (abstinent for 3 months), presented with acute bilateral lower extremity edema and diffuse petechiae. Vitals were within normal limits and exam revealed diffuse jaundice, scleral icterus, scattered ecchymoses on his extremities and flanks, with bilateral pitting edema. Labs were remarkable for anemia (Hb 11.5g/dL), thrombocytopenia (PLT 87K/mm3). hyponatremia (132mEq/L), hypokalemia (3.1mEq/L), abnormal LFT’s (ALP 226 U/L, AST 156 U/L, ALT 86 U/L), and conjugated hyperbilirubinemia (Tbili 55.2mg/dL, Dbili 31.8mg/dL). MDF was 84.6. An extensive hepatitis workup was unremarkable. Abdominal U/S revealed a nodular and echogenic liver of 19.8 cm. CT confirmed cirrhosis with evidence for portal hypertension and splenomegaly. He was admitted for suspected AH and treated with a 7-day course of prednisolone 40 mg daily. Further workup revealed hemosiderinuria, low haptoglobin, and positive IIb/IIIa antibodies, concerning for ITP. Labs were repeated one month following discharge and he was continued on steroids for a total of 48-days with taper. He was seen in office with resolution of his ITP and presumed AH, with a total bilirubin of 1.9 mg/dL.
Discussion: Our patient was treated for ITP and concomitant AH with prednisolone, although a definitive diagnosis could not be made. His bilirubin and platelets improved with this treatment at a dosing of 1 mg/kg, which is the regimen for ITP, albeit at one-half of the suggested duration. Due to the complexity of his presentation, determining the optimal management for this patient was difficult. It is important for clinicians to remember the broad differentials of thrombocytopenia and recognize that there may be overlapping etiologies of deranged liver enzymes.
Disclosures:
Brooke E. Kania, DO1, Ariana Tagliaferri, MD2, Dhruv Patel, DO2, Iqra Baig, 2, Alisa Farokhian, MD2. A0580 - Hepatitis With an Unknown Etiology with Concomitant ITP, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1Saint Joseph's University Medical Center, Parsippany-Troy Hills, NJ; 2St. Joseph's University Medical Center, Paterson, NJ
Introduction: Alcoholic hepatitis (AH) usually presents after decades of alcohol consumption and can even manifest with recent abstinence. The clinical presentation may be compounded by underlying liver cirrhosis and LFT’s are not a reliable means of diagnosing AH due to poor sensitivity and specificity. Hepatitis is only one of the major causes of thrombocytopenia. Immune thrombocytopenic purpura (ITP) is a diagnosis of exclusion and further workup is warranted with persistent thrombocytopenia refractory to treatment for AH. Although there is limited data demonstrating a correlation between AH and ITP, both conditions respond to steroids. We present a case of a 42 YO M with an unknown cause of hepatitis and concomitant ITP who responded well to steroids.
Case Description/Methods: A 42 YO M PMH of alcohol use disorder (abstinent for 3 months), presented with acute bilateral lower extremity edema and diffuse petechiae. Vitals were within normal limits and exam revealed diffuse jaundice, scleral icterus, scattered ecchymoses on his extremities and flanks, with bilateral pitting edema. Labs were remarkable for anemia (Hb 11.5g/dL), thrombocytopenia (PLT 87K/mm3). hyponatremia (132mEq/L), hypokalemia (3.1mEq/L), abnormal LFT’s (ALP 226 U/L, AST 156 U/L, ALT 86 U/L), and conjugated hyperbilirubinemia (Tbili 55.2mg/dL, Dbili 31.8mg/dL). MDF was 84.6. An extensive hepatitis workup was unremarkable. Abdominal U/S revealed a nodular and echogenic liver of 19.8 cm. CT confirmed cirrhosis with evidence for portal hypertension and splenomegaly. He was admitted for suspected AH and treated with a 7-day course of prednisolone 40 mg daily. Further workup revealed hemosiderinuria, low haptoglobin, and positive IIb/IIIa antibodies, concerning for ITP. Labs were repeated one month following discharge and he was continued on steroids for a total of 48-days with taper. He was seen in office with resolution of his ITP and presumed AH, with a total bilirubin of 1.9 mg/dL.
Discussion: Our patient was treated for ITP and concomitant AH with prednisolone, although a definitive diagnosis could not be made. His bilirubin and platelets improved with this treatment at a dosing of 1 mg/kg, which is the regimen for ITP, albeit at one-half of the suggested duration. Due to the complexity of his presentation, determining the optimal management for this patient was difficult. It is important for clinicians to remember the broad differentials of thrombocytopenia and recognize that there may be overlapping etiologies of deranged liver enzymes.
Disclosures:
Brooke Kania indicated no relevant financial relationships.
Ariana Tagliaferri indicated no relevant financial relationships.
Dhruv Patel indicated no relevant financial relationships.
Iqra Baig indicated no relevant financial relationships.
Alisa Farokhian indicated no relevant financial relationships.
Brooke E. Kania, DO1, Ariana Tagliaferri, MD2, Dhruv Patel, DO2, Iqra Baig, 2, Alisa Farokhian, MD2. A0580 - Hepatitis With an Unknown Etiology with Concomitant ITP, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
