Back


Poster Session A - Sunday Afternoon
Category: Colon
A0158 - A Segmental Colitis Associated With Diverticulosis versus Inflammatory Bowel Disease: A Diagnostic Dilemma Despite Total Proctocolectomy
Sunday, October 23, 2022
5:00 PM – 7:00 PM ET
Location: Crown Ballroom

Has Audio
- AM
Amrendra Mandal, MD
SUNY Upstate Medical University
Syracuse, NY
Presenting Author(s)
Amrendra Mandal, MD1, Vijay Gayam, MD2, Amanda Eisinger, DO1, Gayatri Pemmasani, MD1, James Osei Sarpong, MD1, Ganesh Aswath, MD1
1SUNY Upstate Medical University, Syracuse, NY; 2The Brooklyn Hospital Center, Brooklyn, NY
Introduction: Patients with diverticular disease can develop segmental colitis associated with diverticulosis (SCAD). It can range from mild inflammatory changes to chronic active inflammation that mimics inflammatory bowel disease (IBD). SCAD usually presents a more benign outcome, with a low rate of complications. Here, we present a complex case in which a diagnosis was still unclear till the final stage of the management.
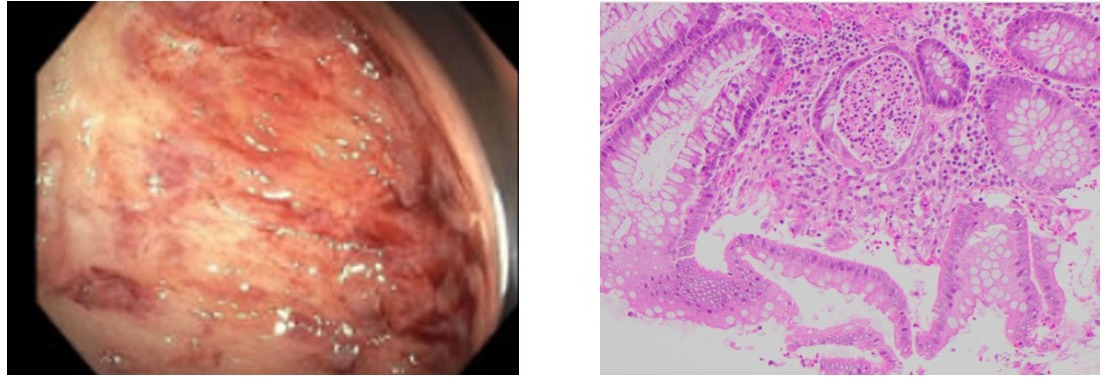
Case Description/Methods: A 60-year-old female was admitted for hypovolemic shock. She was resuscitated, and the GI was consulted for the management of IBD. She was recently diagnosed with ulcerative colitis about two months ago. She has abdominal pain in the right lower side, and examination revealed mild abdominal tenderness. She was already on prednisone 60 mg daily for two weeks and infliximab maintenance dose (completed two doses) and mesalamine from the last admission. She has had three colonoscopies in the past. The first colonoscopy six months ago showed a normal rectum, unable to traverse the sigmoid colon due to stricture and diverticulosis. The biopsy showed a normal rectum and a very focal area of cryptitis. The last colonoscopy two months ago showed a severely inflamed ulcerated mucosa in the sigmoid colon (figure 1). Colon biopsy showed mild acute cryptitis and distorted and branched crypts. No crypt abscesses or granulomas were seen. On this admission, CT enterography showed pancolitis. Serology for Crohn's disease (CD) was negative, including ASCA IgA and ASCA IgG. The strong differential diagnosis was SCAD vs.IBD. The decision was to continue with the medical treatment (i.e., completion of steroid course, infliximab, and follow the response) and was discharged. The patient again presented with a shock one month after this admission. Unfortunately, she had colonic perforation and had total proctocolectomy with ileostomy creation. Pathology of surgical specimens revealed mild chronic active colitis and severe diverticular disease with associated transmural inflammation (figure 2). Ileum excision showed no significant pathologic changes unlikely to be CD. The patient was doing well till the last follow-up.
Discussion: This is a unique case where the diagnosis of SCAD vs. IBD was unclear regardless of the availability of serology, endoscopic, surgery, and histopathological examinations. In this complex case, we suggest a multidisciplinary team approach to improve patient-centered care.
Disclosures:
Amrendra Mandal, MD1, Vijay Gayam, MD2, Amanda Eisinger, DO1, Gayatri Pemmasani, MD1, James Osei Sarpong, MD1, Ganesh Aswath, MD1. A0158 - A Segmental Colitis Associated With Diverticulosis versus Inflammatory Bowel Disease: A Diagnostic Dilemma Despite Total Proctocolectomy, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1SUNY Upstate Medical University, Syracuse, NY; 2The Brooklyn Hospital Center, Brooklyn, NY
Introduction: Patients with diverticular disease can develop segmental colitis associated with diverticulosis (SCAD). It can range from mild inflammatory changes to chronic active inflammation that mimics inflammatory bowel disease (IBD). SCAD usually presents a more benign outcome, with a low rate of complications. Here, we present a complex case in which a diagnosis was still unclear till the final stage of the management.
Case Description/Methods: A 60-year-old female was admitted for hypovolemic shock. She was resuscitated, and the GI was consulted for the management of IBD. She was recently diagnosed with ulcerative colitis about two months ago. She has abdominal pain in the right lower side, and examination revealed mild abdominal tenderness. She was already on prednisone 60 mg daily for two weeks and infliximab maintenance dose (completed two doses) and mesalamine from the last admission. She has had three colonoscopies in the past. The first colonoscopy six months ago showed a normal rectum, unable to traverse the sigmoid colon due to stricture and diverticulosis. The biopsy showed a normal rectum and a very focal area of cryptitis. The last colonoscopy two months ago showed a severely inflamed ulcerated mucosa in the sigmoid colon (figure 1). Colon biopsy showed mild acute cryptitis and distorted and branched crypts. No crypt abscesses or granulomas were seen. On this admission, CT enterography showed pancolitis. Serology for Crohn's disease (CD) was negative, including ASCA IgA and ASCA IgG. The strong differential diagnosis was SCAD vs.IBD. The decision was to continue with the medical treatment (i.e., completion of steroid course, infliximab, and follow the response) and was discharged. The patient again presented with a shock one month after this admission. Unfortunately, she had colonic perforation and had total proctocolectomy with ileostomy creation. Pathology of surgical specimens revealed mild chronic active colitis and severe diverticular disease with associated transmural inflammation (figure 2). Ileum excision showed no significant pathologic changes unlikely to be CD. The patient was doing well till the last follow-up.
Discussion: This is a unique case where the diagnosis of SCAD vs. IBD was unclear regardless of the availability of serology, endoscopic, surgery, and histopathological examinations. In this complex case, we suggest a multidisciplinary team approach to improve patient-centered care.
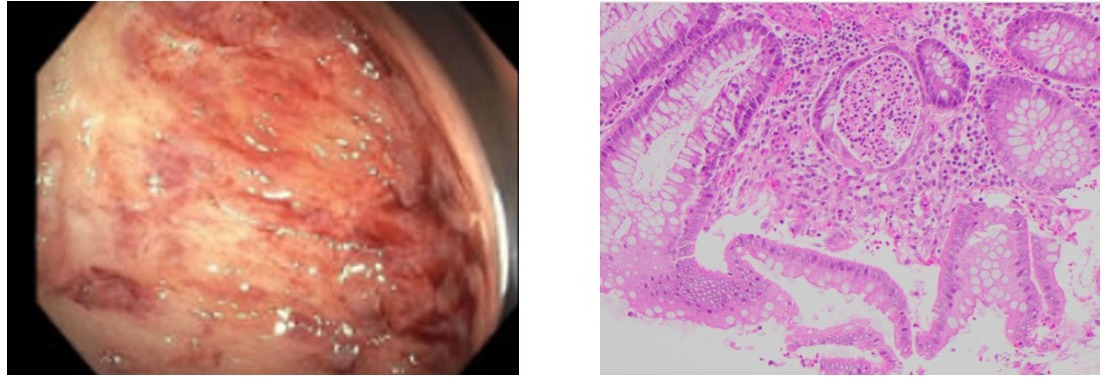
Figure: figure 1, figure 2
Disclosures:
Amrendra Mandal indicated no relevant financial relationships.
Vijay Gayam indicated no relevant financial relationships.
Amanda Eisinger indicated no relevant financial relationships.
Gayatri Pemmasani indicated no relevant financial relationships.
James Osei Sarpong indicated no relevant financial relationships.
Ganesh Aswath indicated no relevant financial relationships.
Amrendra Mandal, MD1, Vijay Gayam, MD2, Amanda Eisinger, DO1, Gayatri Pemmasani, MD1, James Osei Sarpong, MD1, Ganesh Aswath, MD1. A0158 - A Segmental Colitis Associated With Diverticulosis versus Inflammatory Bowel Disease: A Diagnostic Dilemma Despite Total Proctocolectomy, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
