Back

Poster Session A - Sunday Afternoon
Category: Functional Bowel Disease
A0263 - Neurogastroenterology & Motility Manifestations After COVID-19 Infection: A Case Series
Sunday, October 23, 2022
5:00 PM – 7:00 PM ET
Location: Crown Ballroom
Has Audio

Saad Javed, MD
Allegheny Health Network
Grove City, Pennsylvania
Presenting Author(s)
Saad Javed, MD
Allegheny Health Network, Grove City, PA
Introduction: In a subset of Covid19-convalescent patients, a multitude of long-term sequelae are increasingly being reported.
We report four cases with varying neuro-GI and motility manifestations after recent COVID-19 infection.
Case Description/Methods: Case 1:
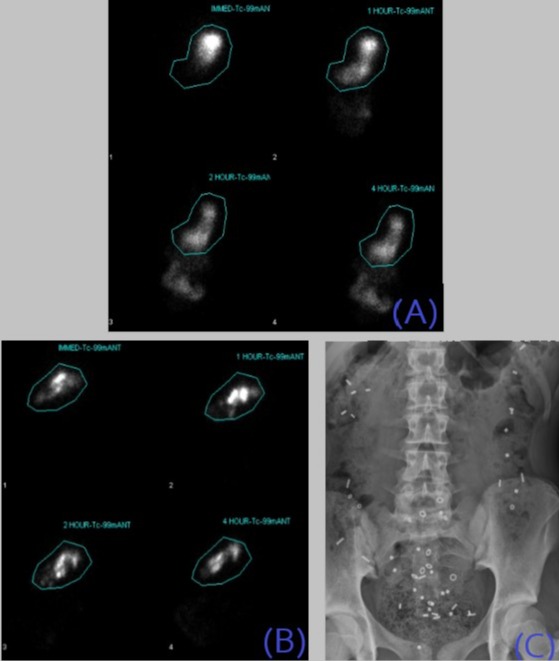
23 year old man contracted Covid-19 and had a protracted course of respiratory illness. Despite resolution of respiratory symptoms and dysgeusia, he continued to experience early satiety, postprandial nausea, vomiting and unintentional weight loss. Gastric Emptying Scan (GES) revealed gastroparesis (figure A). Dietary modification and metoclopramide led to symptomatic improvement.
Case 2:
39 year old woman with migraines, suffered from Covid-19 infection where anosmia and respiratory symptoms lasted for two weeks. Despite resolution of initial symptoms, she started experiencing nausea and vomiting, and reported stereotypical symptoms with complete absence of vomiting between episodes. Endoscopic examination, CT head and GES were normal. Urine tox screen was negative for cannabinoids. She responded favorably to amitriptyline and ondansetron.
Case 3:
47 year old man started experiencing severe constipation associated with abdominal pain and bloating soon after being diagnosed with Covid-19. Three months after resolution of respiratory symptoms, in addition to constipation, he began reporting postprandial fullness, early satiation and epigastric pain. GES showed gastroparesis (figure B) and a Sitzmarks® Study revealed delayed colonic transit (figure C). Prucalopride was started, leading to improvement in symptoms.
Case 4:
74 year old woman with obesity and diabetes, was hospitalized and intubated for severe respiratory distress due to Covid-19. After discharge, she had persistent symptoms of brain fog, fatigue, dyspnea as well as diarrhea and abdominal cramping, persisting despite loperamide and dicyclomine. C.difficile toxin, random colonic biopsies and H2 breath test were unremarkable. Her symptoms eventually improved with rifaximin.
Discussion: We report four cases with post-Covid gastroparesis, cyclical vomiting syndrome, pan-gut dysmotility, and post-infectious IBS phenotypes.The pathophysiology of post-infectious-gut–brain disorders is still obscure. The current conceptual framework implicates acquired neuropathy, altered motility, intestinal barrier disruption and persistent intestinal inflammation.
Similar pathophysiology may be involved in COVID-19 infection leading to sustained neurogastroenterological dysfunction and gut dysmotility.
Disclosures:
Saad Javed, MD. A0263 - Neurogastroenterology & Motility Manifestations After COVID-19 Infection: A Case Series, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
Allegheny Health Network, Grove City, PA
Introduction: In a subset of Covid19-convalescent patients, a multitude of long-term sequelae are increasingly being reported.
We report four cases with varying neuro-GI and motility manifestations after recent COVID-19 infection.
Case Description/Methods: Case 1:
23 year old man contracted Covid-19 and had a protracted course of respiratory illness. Despite resolution of respiratory symptoms and dysgeusia, he continued to experience early satiety, postprandial nausea, vomiting and unintentional weight loss. Gastric Emptying Scan (GES) revealed gastroparesis (figure A). Dietary modification and metoclopramide led to symptomatic improvement.
Case 2:
39 year old woman with migraines, suffered from Covid-19 infection where anosmia and respiratory symptoms lasted for two weeks. Despite resolution of initial symptoms, she started experiencing nausea and vomiting, and reported stereotypical symptoms with complete absence of vomiting between episodes. Endoscopic examination, CT head and GES were normal. Urine tox screen was negative for cannabinoids. She responded favorably to amitriptyline and ondansetron.
Case 3:
47 year old man started experiencing severe constipation associated with abdominal pain and bloating soon after being diagnosed with Covid-19. Three months after resolution of respiratory symptoms, in addition to constipation, he began reporting postprandial fullness, early satiation and epigastric pain. GES showed gastroparesis (figure B) and a Sitzmarks® Study revealed delayed colonic transit (figure C). Prucalopride was started, leading to improvement in symptoms.
Case 4:
74 year old woman with obesity and diabetes, was hospitalized and intubated for severe respiratory distress due to Covid-19. After discharge, she had persistent symptoms of brain fog, fatigue, dyspnea as well as diarrhea and abdominal cramping, persisting despite loperamide and dicyclomine. C.difficile toxin, random colonic biopsies and H2 breath test were unremarkable. Her symptoms eventually improved with rifaximin.
Discussion: We report four cases with post-Covid gastroparesis, cyclical vomiting syndrome, pan-gut dysmotility, and post-infectious IBS phenotypes.The pathophysiology of post-infectious-gut–brain disorders is still obscure. The current conceptual framework implicates acquired neuropathy, altered motility, intestinal barrier disruption and persistent intestinal inflammation.
Similar pathophysiology may be involved in COVID-19 infection leading to sustained neurogastroenterological dysfunction and gut dysmotility.
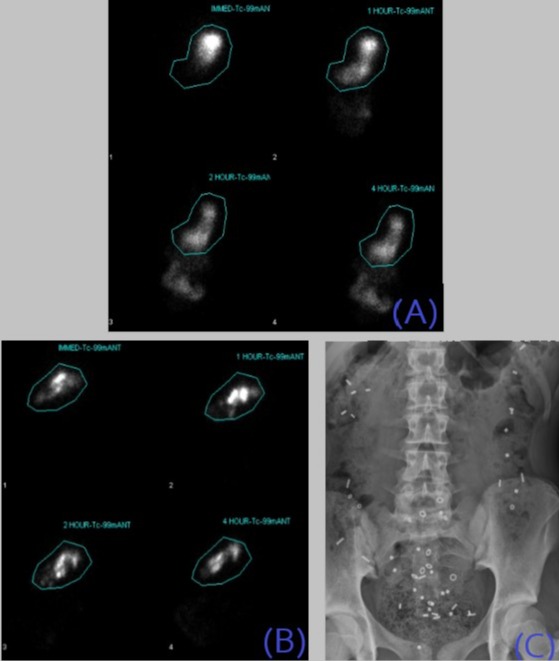
Figure: Image (A) showing delayed gastric emptying with 64% retention at 4 hours.
Images (B) and (C) both from Case-3 showing markedly delayed gastric emptying with 86% retention at 4 hours and abnormal colonic transit study with X-ray showing large amount of stool and retention of markers throughout the entire colon, in the same patient.
Images (B) and (C) both from Case-3 showing markedly delayed gastric emptying with 86% retention at 4 hours and abnormal colonic transit study with X-ray showing large amount of stool and retention of markers throughout the entire colon, in the same patient.
Disclosures:
Saad Javed indicated no relevant financial relationships.
Saad Javed, MD. A0263 - Neurogastroenterology & Motility Manifestations After COVID-19 Infection: A Case Series, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
