Back

Poster Session A - Sunday Afternoon
Category: Esophagus
A0232 - A Rare Finding of a Common Disorder
Sunday, October 23, 2022
5:00 PM – 7:00 PM ET
Location: Crown Ballroom
Has Audio
- SN
Sandra Naffouj, MD
University of Illinois at Chicago
Chicago, IL
Presenting Author(s)
Sandra Naffouj, MD1, Elie Ghoulam, MD2, Meredith Yellen, MD1, Robert E. Carroll, MD1
1University of Illinois at Chicago, Chicago, IL; 2University of Ilinois at Chicago, Chicago, IL
Introduction: Esophagitis dissecans superficialis (EDS) is a rare desquamative disorder of the esophagus, characterized by sloughing of the esophageal squamous mucosa. Most cases of EDS have been associated with autoimmune bullous dermatoses, medications like bisphosphonates, chemical irritants, iatrogenic injury, and celiac disease. To our knowledge, EDS has not previously been reported with achalasia.
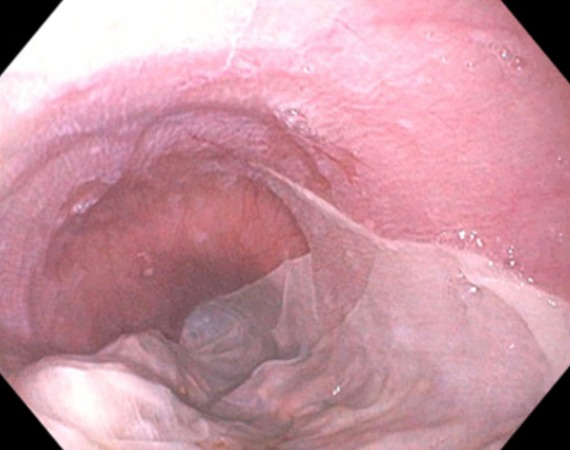
Case Description/Methods: Our patient is a 42-year-old woman with Hashimoto’s thyroiditis and untreated achalasia type II diagnosed on high-resolution manometry four years ago who presented to the hospital with dysphagia to both solids and liquids and oral intake intolerance for one week. She also endorsed weight loss, nausea, and vomiting clear secretions mixed with thick white cord-like material. Physical exam was remarkable for dry mucous membranes. Laboratory tests were notable for mild leukocytosis. Given her history of achalasia and progressive symptoms, esophagogastroduodenoscopy (EGD) was performed and showed large fragments of mucosal sloughing in the distal esophagus or “tissue paper esophagus” consistent with EDS and hypertonic lower esophageal sphincter (Image 1). Pneumatic dilation (PD) to 30 mm was successfully performed with improvement in symptoms. She was continued on a daily proton pump inhibitor and was doing well on her 4-month follow-up.
Discussion: EDS can be an incidental finding on endoscopy or can present with a variety of symptoms, including dysphagia, odynophagia, coughing, or vomiting the sloughed esophageal mucosa like in our patient. The pathogenesis remains unclear. It might represent a mucosal reaction to various insults (iatrogenic, chemical, thermal, and immunological). Although EDS has been reported in association with certain dermatologic and gastrointestinal autoimmune diseases like celiac disease, it has not been reported in the setting of achalasia. Perhaps the possible autoimmune pathogenesis of achalasia related to antibodies against the enteric neurons contributes to its occurrence. Biopsies are recommended to rule out other etiologies such as candidiasis and squamous cell carcinoma (SCC). There is no specific treatment for EDS; a combination of acid suppression and discontinuation of the offending agent if present can result in healing. Prognosis is benign without lasting esophageal complications. In conclusion, endoscopists need to be aware of EDS in order not to mistake it for other conditions like esophagitis and SCC and to recognize its association with achalasia.
Disclosures:
Sandra Naffouj, MD1, Elie Ghoulam, MD2, Meredith Yellen, MD1, Robert E. Carroll, MD1. A0232 - A Rare Finding of a Common Disorder, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1University of Illinois at Chicago, Chicago, IL; 2University of Ilinois at Chicago, Chicago, IL
Introduction: Esophagitis dissecans superficialis (EDS) is a rare desquamative disorder of the esophagus, characterized by sloughing of the esophageal squamous mucosa. Most cases of EDS have been associated with autoimmune bullous dermatoses, medications like bisphosphonates, chemical irritants, iatrogenic injury, and celiac disease. To our knowledge, EDS has not previously been reported with achalasia.
Case Description/Methods: Our patient is a 42-year-old woman with Hashimoto’s thyroiditis and untreated achalasia type II diagnosed on high-resolution manometry four years ago who presented to the hospital with dysphagia to both solids and liquids and oral intake intolerance for one week. She also endorsed weight loss, nausea, and vomiting clear secretions mixed with thick white cord-like material. Physical exam was remarkable for dry mucous membranes. Laboratory tests were notable for mild leukocytosis. Given her history of achalasia and progressive symptoms, esophagogastroduodenoscopy (EGD) was performed and showed large fragments of mucosal sloughing in the distal esophagus or “tissue paper esophagus” consistent with EDS and hypertonic lower esophageal sphincter (Image 1). Pneumatic dilation (PD) to 30 mm was successfully performed with improvement in symptoms. She was continued on a daily proton pump inhibitor and was doing well on her 4-month follow-up.
Discussion: EDS can be an incidental finding on endoscopy or can present with a variety of symptoms, including dysphagia, odynophagia, coughing, or vomiting the sloughed esophageal mucosa like in our patient. The pathogenesis remains unclear. It might represent a mucosal reaction to various insults (iatrogenic, chemical, thermal, and immunological). Although EDS has been reported in association with certain dermatologic and gastrointestinal autoimmune diseases like celiac disease, it has not been reported in the setting of achalasia. Perhaps the possible autoimmune pathogenesis of achalasia related to antibodies against the enteric neurons contributes to its occurrence. Biopsies are recommended to rule out other etiologies such as candidiasis and squamous cell carcinoma (SCC). There is no specific treatment for EDS; a combination of acid suppression and discontinuation of the offending agent if present can result in healing. Prognosis is benign without lasting esophageal complications. In conclusion, endoscopists need to be aware of EDS in order not to mistake it for other conditions like esophagitis and SCC and to recognize its association with achalasia.
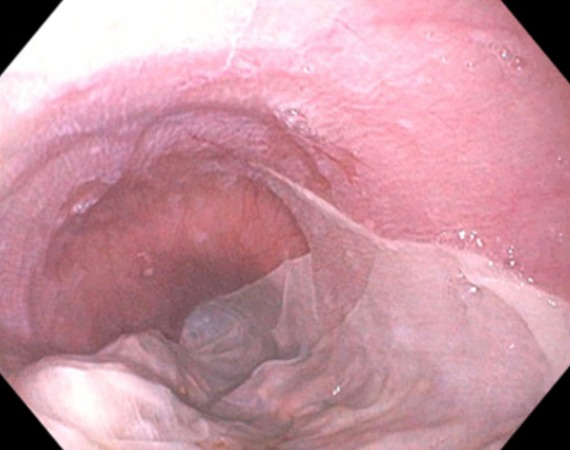
Figure: Sloughing of the esophageal mucosa described as "tissue paper esophagus" in esophagitis dissecans superficialis.
Disclosures:
Sandra Naffouj indicated no relevant financial relationships.
Elie Ghoulam indicated no relevant financial relationships.
Meredith Yellen indicated no relevant financial relationships.
Robert Carroll indicated no relevant financial relationships.
Sandra Naffouj, MD1, Elie Ghoulam, MD2, Meredith Yellen, MD1, Robert E. Carroll, MD1. A0232 - A Rare Finding of a Common Disorder, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
