Back

Poster Session A - Sunday Afternoon
Category: Biliary/Pancreas
A0044 - Application of Endoscopic Powered Resection (EPR) in Pancreatic Necrosectomy Post Cystogastrostomy
Sunday, October 23, 2022
5:00 PM – 7:00 PM ET
Location: Crown Ballroom
Has Audio

Pranay Reddy, MD, MPH
Jefferson Health Northeast
Philadelphia, PA
Presenting Author(s)
Pranay Reddy, MD, MPH1, David Valadez, MD2, Mojtaba Olyaee, MD, FACG3, Richard Sutton, DO4
1Jefferson Health Northeast, Philadelphia, PA; 2University of Kansas Medical Center, Kansas City, KS; 3University of Kansas Medical Center, Leawood, KS; 4Kansas University Medical Center, Kansas City, KS
Introduction: Patients with severe pancreatitis routinely develop walled off necrotic collections that require a procedure known as a Cystogastrostomy. This procedure creates an opening between the necrotic collection and the stomach to help facilitate removal of necrotic tissue. Serial endoscopic necrosectomies are often required to remove all the necrotic debris. Endoscopic powered resection (EPR) is a procedure used to perform mechanical mucosectomies of polyps within the gastrointestinal tract. This method of mechanical resection has recently been applied to endoscopic pancreatic necrosectomy and debridement. The following case highlights a novel application of EPR in performing pancreatic necrosectomies following cystogastrostomy to help decrease the number of repeat procedures.
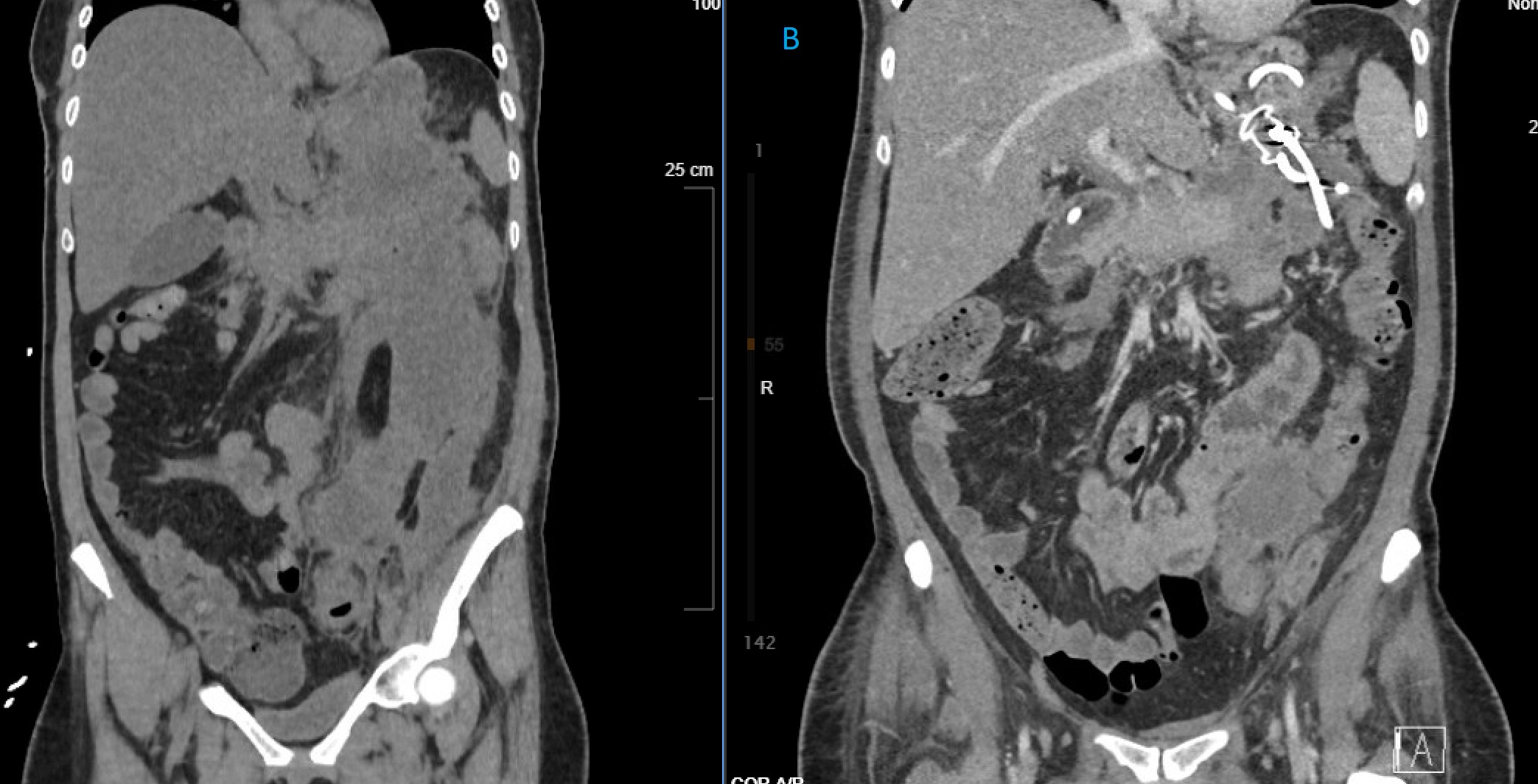
Case Description/Methods: A 47-year-old patient with past medical history of asthma, hyperlipidemia, breast cancer, recent hypertriglyceridemia-induced acute pancreatitis initially presented with fevers, chills and abdominal pain. Initial labs remarkable for leukocytosis WBC 19.7 K/UL. CT scan showed concern for new infected peripancreatic necrotic fluid collection measuring 9.5 x 6.0 cm extending inferiorly along the left paracolic gutter. An EUS with cystogastrostomy and endoluminal stent placement was performed to facilitate drainage of the necrotic collection. Repeat EGD with both EPR and snare necrosectomy was performed the following week. CT scan completed two days later showed marked interval decrease in the multiloculated peripherally enhancing peripancreatic air and fluid collection now measuring 7.3 x 4.0 cm. The patient underwent second necrosectomy one week later with EPR and snare mechanical debridement which revealed an 18 cm cyst cavity. Significant amount of necrotic tissue removed at that time and patient scheduled for repeat EGD in 3 weeks with endoluminal stent retreatment.
Discussion: Endoscopic pancreatic necrosectomy is often performed 4 weeks after the initial episode of pancreatitis to allow formation of a true, walled off necrotic collection. When performing endoscopic necrosectomy of large collections, at least 5 procedures are often required to completely removal all necrotic tissue. As shown in this case, implementation of EPR with traditional endoscopic snare necrosectomy can facilitate efficient removal of debris and help decrease the number of repeat necrosectomies. This could ultimately improve resource utilization and have major implications on overall patient morbidity and mortality.
Disclosures:
Pranay Reddy, MD, MPH1, David Valadez, MD2, Mojtaba Olyaee, MD, FACG3, Richard Sutton, DO4. A0044 - Application of Endoscopic Powered Resection (EPR) in Pancreatic Necrosectomy Post Cystogastrostomy, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1Jefferson Health Northeast, Philadelphia, PA; 2University of Kansas Medical Center, Kansas City, KS; 3University of Kansas Medical Center, Leawood, KS; 4Kansas University Medical Center, Kansas City, KS
Introduction: Patients with severe pancreatitis routinely develop walled off necrotic collections that require a procedure known as a Cystogastrostomy. This procedure creates an opening between the necrotic collection and the stomach to help facilitate removal of necrotic tissue. Serial endoscopic necrosectomies are often required to remove all the necrotic debris. Endoscopic powered resection (EPR) is a procedure used to perform mechanical mucosectomies of polyps within the gastrointestinal tract. This method of mechanical resection has recently been applied to endoscopic pancreatic necrosectomy and debridement. The following case highlights a novel application of EPR in performing pancreatic necrosectomies following cystogastrostomy to help decrease the number of repeat procedures.
Case Description/Methods: A 47-year-old patient with past medical history of asthma, hyperlipidemia, breast cancer, recent hypertriglyceridemia-induced acute pancreatitis initially presented with fevers, chills and abdominal pain. Initial labs remarkable for leukocytosis WBC 19.7 K/UL. CT scan showed concern for new infected peripancreatic necrotic fluid collection measuring 9.5 x 6.0 cm extending inferiorly along the left paracolic gutter. An EUS with cystogastrostomy and endoluminal stent placement was performed to facilitate drainage of the necrotic collection. Repeat EGD with both EPR and snare necrosectomy was performed the following week. CT scan completed two days later showed marked interval decrease in the multiloculated peripherally enhancing peripancreatic air and fluid collection now measuring 7.3 x 4.0 cm. The patient underwent second necrosectomy one week later with EPR and snare mechanical debridement which revealed an 18 cm cyst cavity. Significant amount of necrotic tissue removed at that time and patient scheduled for repeat EGD in 3 weeks with endoluminal stent retreatment.
Discussion: Endoscopic pancreatic necrosectomy is often performed 4 weeks after the initial episode of pancreatitis to allow formation of a true, walled off necrotic collection. When performing endoscopic necrosectomy of large collections, at least 5 procedures are often required to completely removal all necrotic tissue. As shown in this case, implementation of EPR with traditional endoscopic snare necrosectomy can facilitate efficient removal of debris and help decrease the number of repeat necrosectomies. This could ultimately improve resource utilization and have major implications on overall patient morbidity and mortality.
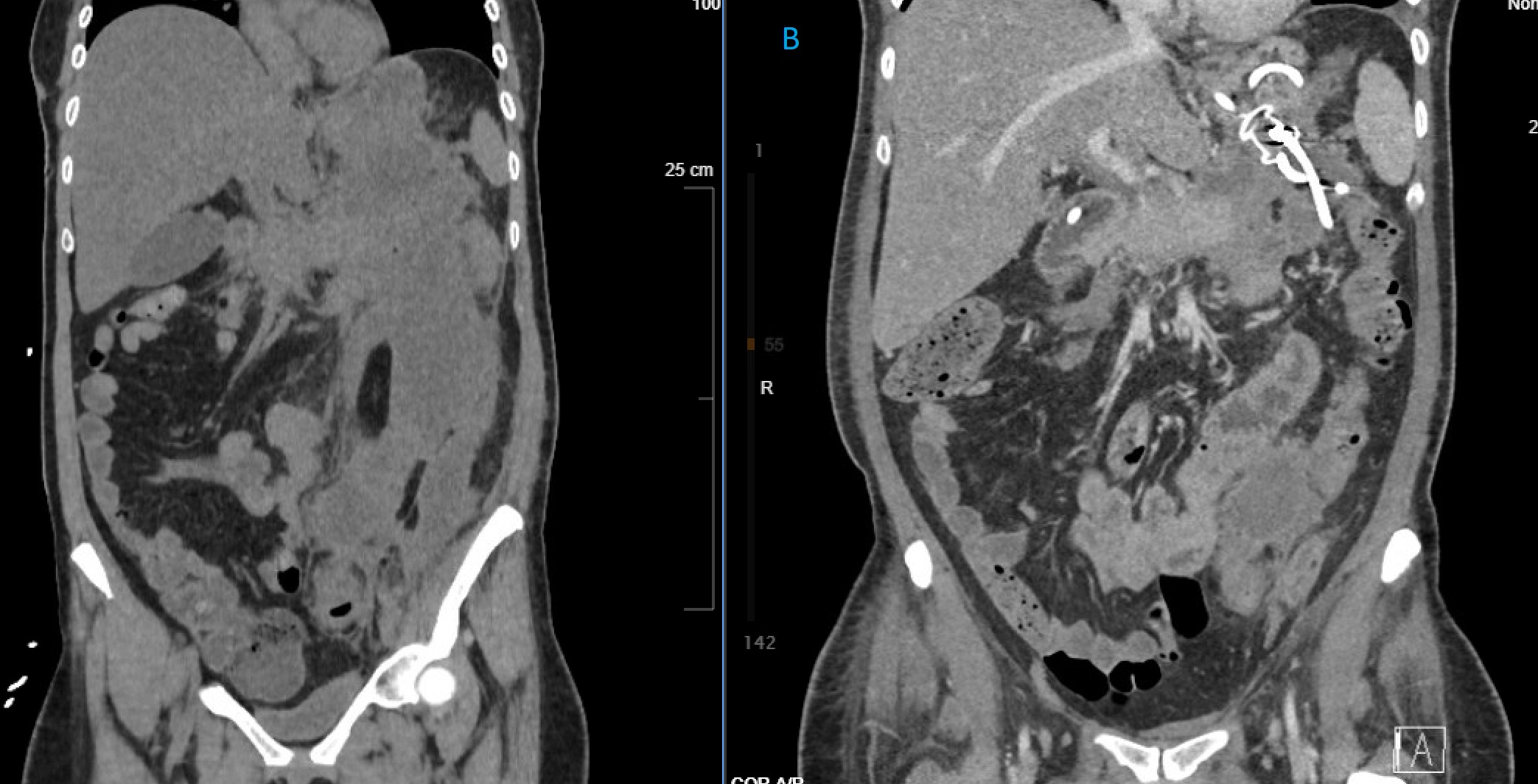
Figure: A. Large (9.5 x 6.0 cm) peripancreatic necrotic fluid collection with inferior extension into left paracolic gutter
B. Marked interval decrease in multiloculated necrotic collection following second EPR necrosectomy with endoluminal stent visualized.
B. Marked interval decrease in multiloculated necrotic collection following second EPR necrosectomy with endoluminal stent visualized.
Disclosures:
Pranay Reddy indicated no relevant financial relationships.
David Valadez indicated no relevant financial relationships.
Mojtaba Olyaee indicated no relevant financial relationships.
Richard Sutton indicated no relevant financial relationships.
Pranay Reddy, MD, MPH1, David Valadez, MD2, Mojtaba Olyaee, MD, FACG3, Richard Sutton, DO4. A0044 - Application of Endoscopic Powered Resection (EPR) in Pancreatic Necrosectomy Post Cystogastrostomy, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
