Back

Poster Session C - Monday Afternoon
Category: Small Intestine
C0679 - Hyperlipasemia Due to Duodenal Obstruction Secondary to Gastrostomy Tube Migration
Monday, October 24, 2022
3:00 PM – 5:00 PM ET
Location: Crown Ballroom
Has Audio

Shefali Amin, DO, MSEd
Reading Tower Health
Reading, PA
Presenting Author(s)
Shefali Amin, DO, MSEd1, Parth Desai, DO2, Jesus Salas Noain, MD3, Oluwaseun Shogbesan, MD1, Anish Paudel, MD2, John F. Altomare, MD4
1Reading Tower Health, Reading, PA; 2Tower Health - Reading Hospital, Reading, PA; 3Reading Hospital Tower Health, Reading, PA; 4Digestive Disease Associates, Reading, PA
Introduction: Elevated lipase levels of three or more times the upper limit of normal along with abdominal pain and correlated findings on CT imaging can often diagnose a case of acute pancreatitis. Although uncommon, there are alternative causes of hyperlipasemia not related to acute pancreatitis that clinicians should be aware of. Here we present a case of significantly elevated lipase secondary to duodenal obstruction caused by gastrostomy tube migration.
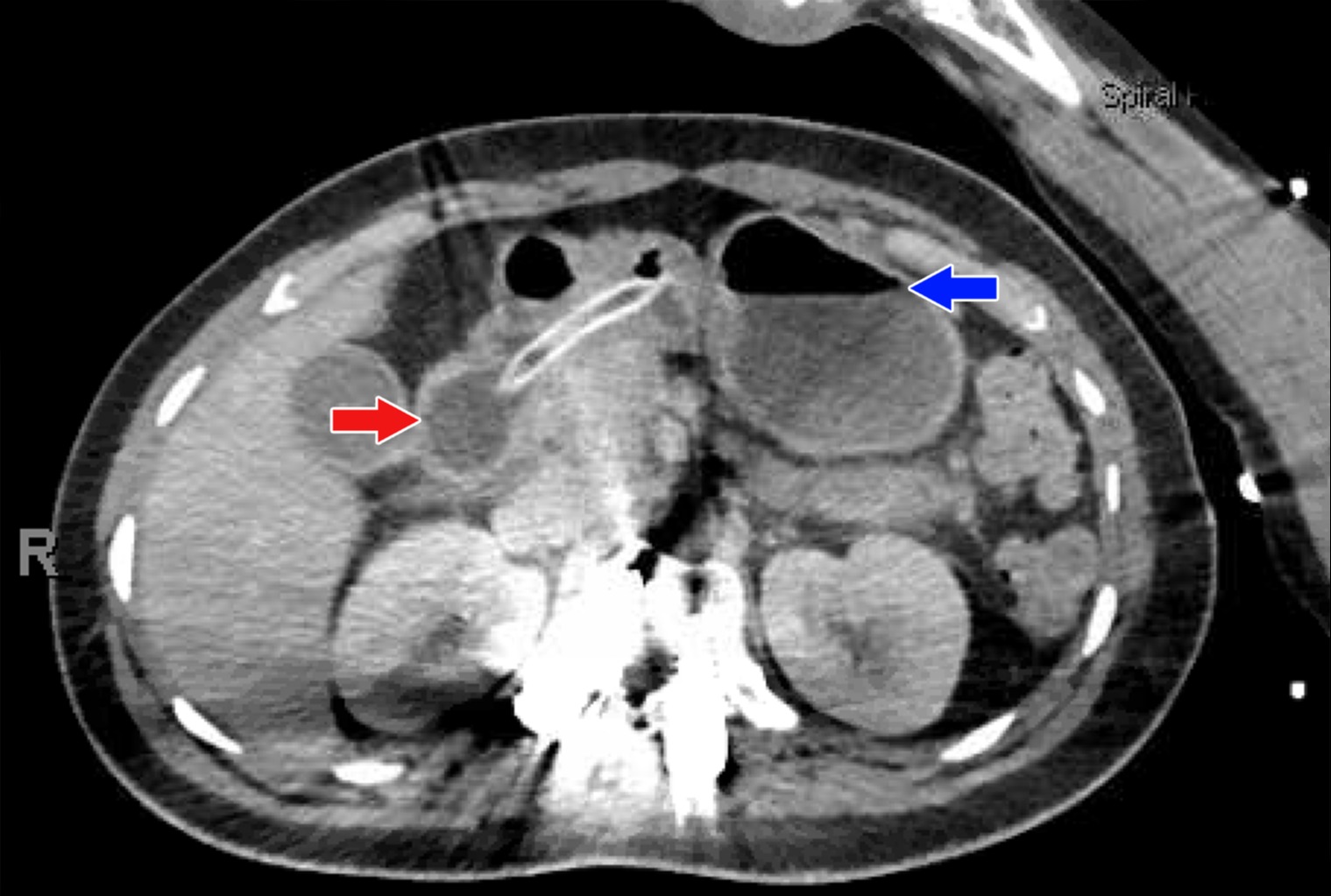
Case Description/Methods: A 30-year-old nonverbal woman with a past medical history of cerebral palsy, refractory grand mal seizures, and chronic (fluoroscopically placed) gastrostomy tube (last changed about one month prior) presented to the hospital for breakthrough seizures, non-bilious vomiting of tube feeds, and abdominal pain. She arrived afebrile with a blood pressure of 165/85 mmHg and otherwise normal vitals. On examination, the patient was nonverbal and appeared uncomfortable with a moderately tender and distended abdomen. The external portion of her gastrostomy tube did not have signs of surrounding infection. Admission laboratory studies were remarkable for a white blood cell count of 13.3 k/ul and lipase of 8216 IU/L. Abdominal CT (Figure 1) showed a normal pancreas, but noted air fluid levels within the stomach as well as the balloon of the percutaneous feeding tube inflated within the second portion of the duodenum, concerning for obstruction. Patient was treated with a nasogastric tube to allow for decompression and the Interventional Radiology service repositioned the gastrostomy tube back into the stomach. After adjustment, the gastrostomy tube placement was confirmed and feeds were re-started. Patient was asymptomatic and tolerating her tube feeds without issue in less than 48 hours from initial presentation.
Discussion: While this case initially appeared to be a straightforward diagnosis of acute pancreatitis, the imaging proved otherwise. Moreover, the patient’s rapid clinical improvement after alleviating the obstruction helped support the alternative diagnosis. It is likely that the obstruction inhibited forward flow of the pancreatic enzymes and instead increased diffusion into the bloodstream causing elevated lipase levels. Clinicians should be aware of the possibility of small bowel obstruction as a cause of hyperlipasemia.
Disclosures:
Shefali Amin, DO, MSEd1, Parth Desai, DO2, Jesus Salas Noain, MD3, Oluwaseun Shogbesan, MD1, Anish Paudel, MD2, John F. Altomare, MD4. C0679 - Hyperlipasemia Due to Duodenal Obstruction Secondary to Gastrostomy Tube Migration, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1Reading Tower Health, Reading, PA; 2Tower Health - Reading Hospital, Reading, PA; 3Reading Hospital Tower Health, Reading, PA; 4Digestive Disease Associates, Reading, PA
Introduction: Elevated lipase levels of three or more times the upper limit of normal along with abdominal pain and correlated findings on CT imaging can often diagnose a case of acute pancreatitis. Although uncommon, there are alternative causes of hyperlipasemia not related to acute pancreatitis that clinicians should be aware of. Here we present a case of significantly elevated lipase secondary to duodenal obstruction caused by gastrostomy tube migration.
Case Description/Methods: A 30-year-old nonverbal woman with a past medical history of cerebral palsy, refractory grand mal seizures, and chronic (fluoroscopically placed) gastrostomy tube (last changed about one month prior) presented to the hospital for breakthrough seizures, non-bilious vomiting of tube feeds, and abdominal pain. She arrived afebrile with a blood pressure of 165/85 mmHg and otherwise normal vitals. On examination, the patient was nonverbal and appeared uncomfortable with a moderately tender and distended abdomen. The external portion of her gastrostomy tube did not have signs of surrounding infection. Admission laboratory studies were remarkable for a white blood cell count of 13.3 k/ul and lipase of 8216 IU/L. Abdominal CT (Figure 1) showed a normal pancreas, but noted air fluid levels within the stomach as well as the balloon of the percutaneous feeding tube inflated within the second portion of the duodenum, concerning for obstruction. Patient was treated with a nasogastric tube to allow for decompression and the Interventional Radiology service repositioned the gastrostomy tube back into the stomach. After adjustment, the gastrostomy tube placement was confirmed and feeds were re-started. Patient was asymptomatic and tolerating her tube feeds without issue in less than 48 hours from initial presentation.
Discussion: While this case initially appeared to be a straightforward diagnosis of acute pancreatitis, the imaging proved otherwise. Moreover, the patient’s rapid clinical improvement after alleviating the obstruction helped support the alternative diagnosis. It is likely that the obstruction inhibited forward flow of the pancreatic enzymes and instead increased diffusion into the bloodstream causing elevated lipase levels. Clinicians should be aware of the possibility of small bowel obstruction as a cause of hyperlipasemia.
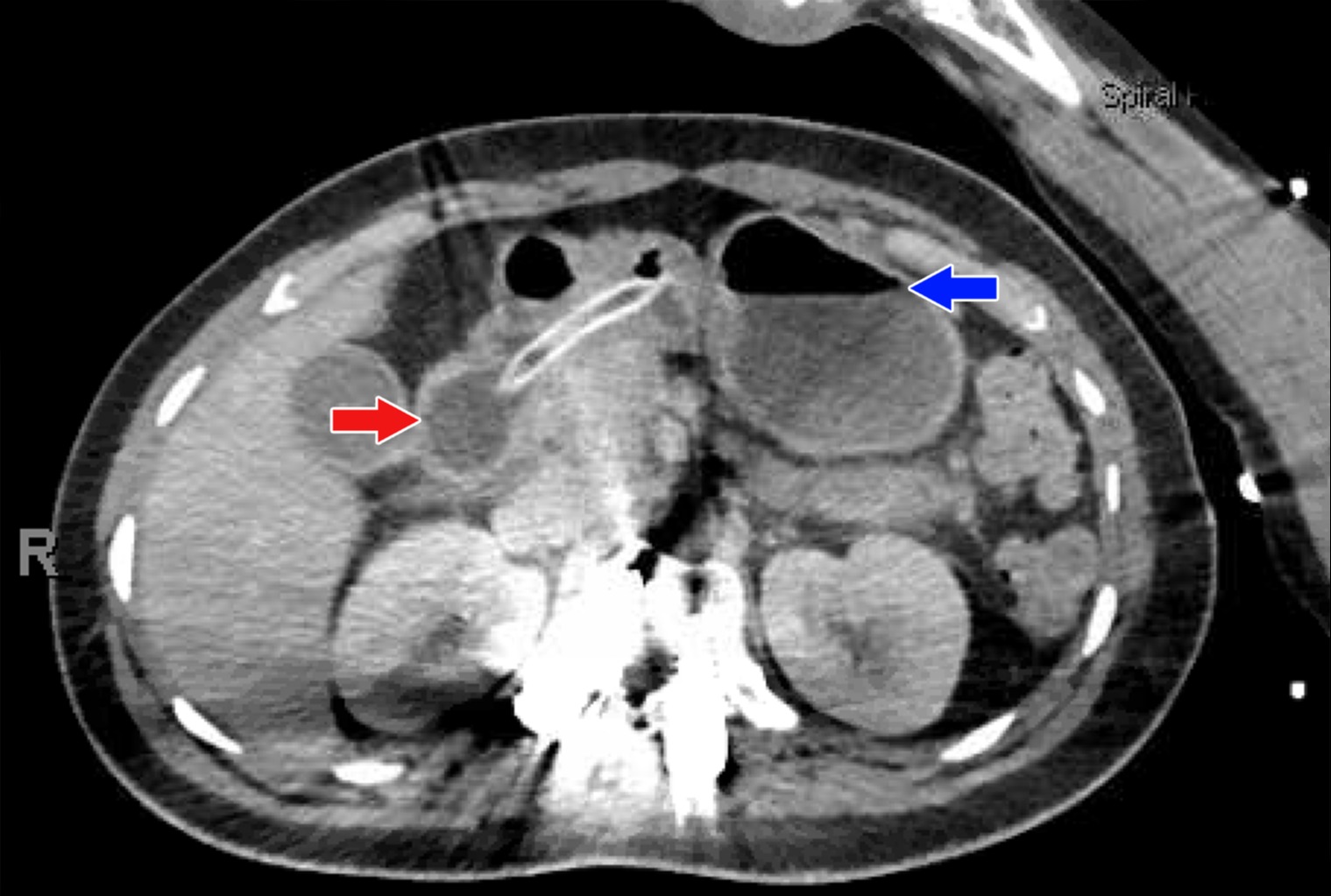
Figure: Caption for Figure 1: CT abdomen showing percutaneous feeding tube with balloon inflated in the second portion of the duodenum (red arrow) and mild fluid level within the stomach (blue arrow).
Disclosures:
Shefali Amin indicated no relevant financial relationships.
Parth Desai indicated no relevant financial relationships.
Jesus Salas Noain indicated no relevant financial relationships.
Oluwaseun Shogbesan indicated no relevant financial relationships.
Anish Paudel indicated no relevant financial relationships.
John Altomare indicated no relevant financial relationships.
Shefali Amin, DO, MSEd1, Parth Desai, DO2, Jesus Salas Noain, MD3, Oluwaseun Shogbesan, MD1, Anish Paudel, MD2, John F. Altomare, MD4. C0679 - Hyperlipasemia Due to Duodenal Obstruction Secondary to Gastrostomy Tube Migration, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
