Back

Poster Session A - Sunday Afternoon
Category: Biliary/Pancreas
A0074 - A Unique Endoscopic Presentation of Intraductal Papillary Mucinous Neoplasms (IPMN) Presenting as a Hemorrhagic Mass
Sunday, October 23, 2022
5:00 PM – 7:00 PM ET
Location: Crown Ballroom
Has Audio
Harsh Patel, MD, MPH
NewYork Presbyterian Brooklyn Methodist Hospital
Brooklyn, NY
Presenting Author(s)
Harsh Patel, MD, MPH1, Sarah Huang, MD1, Dean Rizzi, MD2, Navim Mobin, MD1, Yani Zhao, MD3, Shah Giashuddin, MD4, Mukul Arya, MD5
1NewYork Presbyterian Brooklyn Methodist Hospital, Brooklyn, NY; 2New York Presbyterian Brooklyn Methodist, Brooklyn, NY; 3Long Island Jewish Medical Center at Northwell Health, Queens, NY; 4NYP Brooklyn Methodist Hospital, Brooklyn, NY; 5NewYork-Presbyterian Brooklyn Methodist Hospital, Brooklyn, NY
Introduction: Pancreatic Intraductal papillary mucinous neoplasms (IPMN) are mucinous lesions of the pancreatic duct, accounting for approximately 1% of all pancreatic neoplasms and one fourth of cystic neoplasms. Three types exist: main duct IPMN, branch duct IPMN, and mixed-type IPMN. IPMN is a histologically benign tumor with the potential to be precancerous, and subsequently progress to pancreatic ductal adenocarcinoma. Given the potential of progressing from low-grade dysplasia to invasive carcinoma in approximately 4-6 years, early detection can improve prognosis. They may be asymptomatic or cause abdominal pain, nausea, vomiting, weight loss, jaundice, and pancreatitis. Diagnosis is by CT, MRI, or, in some cases endoscopic ultrasound (EUS) with fine needle aspiration (FNA), followed by biochemical and histopathological analysis.
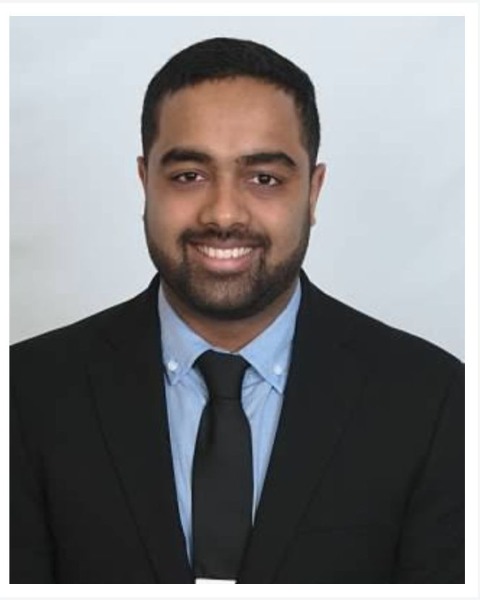
Case Description/Methods: We report a 45 year old female with a history of hypertension, who presented to our hospital after outside imaging showed a pancreatic mass on CT abdomen and pelvis. EUS was performed, which showed an irregular, 10-mm mass with well-defined borders in the main pancreatic duct. There was no abnormality of the common bile duct and no stones identified. The patient subsequently underwent an ERCP one month later, which showed moderate dilation of both the ventral pancreatic duct in the head of pancreas and main pancreatic duct. A 12-15 mm hemorrhagic “cauliflower” mass was also found which was oozing and friable. Biopsy was consistent with intraductal papillary mucinous neoplasm. The patient subsequently underwent a successful Whipple procedure. Surgical pathology returned showing intra-ampullary papillary tubular neoplasms (IAPN) with high grade dysplasia, and resection margins negative for neoplasm.
Discussion: With technological advancements in radiographic and endoscopic imaging, the incidence of IPMN has increased. CT fish mouth ampulla sign (continuous water attenuation from the pancreatic duct to the duodenal lumen) and endoscopic fish mouth ampulla (E-FMA) signs are highly specific for main duct and mixed IPMN. Our patient’s findings are unique in that her ERCP showed a hemorrhagic mass representing an unusual presentation of a common pancreatic lesion. Additionally, we aim to illustrate the importance of early endoscopic evaluation with endoscopy in patients with pancreatic changes on cross sectional imaging. The malignant potential for main duct IPMN is greater than for branch and mixed type IPMNs and therefore more commonly surgically resected.
Disclosures:
Harsh Patel, MD, MPH1, Sarah Huang, MD1, Dean Rizzi, MD2, Navim Mobin, MD1, Yani Zhao, MD3, Shah Giashuddin, MD4, Mukul Arya, MD5. A0074 - A Unique Endoscopic Presentation of Intraductal Papillary Mucinous Neoplasms (IPMN) Presenting as a Hemorrhagic Mass, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1NewYork Presbyterian Brooklyn Methodist Hospital, Brooklyn, NY; 2New York Presbyterian Brooklyn Methodist, Brooklyn, NY; 3Long Island Jewish Medical Center at Northwell Health, Queens, NY; 4NYP Brooklyn Methodist Hospital, Brooklyn, NY; 5NewYork-Presbyterian Brooklyn Methodist Hospital, Brooklyn, NY
Introduction: Pancreatic Intraductal papillary mucinous neoplasms (IPMN) are mucinous lesions of the pancreatic duct, accounting for approximately 1% of all pancreatic neoplasms and one fourth of cystic neoplasms. Three types exist: main duct IPMN, branch duct IPMN, and mixed-type IPMN. IPMN is a histologically benign tumor with the potential to be precancerous, and subsequently progress to pancreatic ductal adenocarcinoma. Given the potential of progressing from low-grade dysplasia to invasive carcinoma in approximately 4-6 years, early detection can improve prognosis. They may be asymptomatic or cause abdominal pain, nausea, vomiting, weight loss, jaundice, and pancreatitis. Diagnosis is by CT, MRI, or, in some cases endoscopic ultrasound (EUS) with fine needle aspiration (FNA), followed by biochemical and histopathological analysis.
Case Description/Methods: We report a 45 year old female with a history of hypertension, who presented to our hospital after outside imaging showed a pancreatic mass on CT abdomen and pelvis. EUS was performed, which showed an irregular, 10-mm mass with well-defined borders in the main pancreatic duct. There was no abnormality of the common bile duct and no stones identified. The patient subsequently underwent an ERCP one month later, which showed moderate dilation of both the ventral pancreatic duct in the head of pancreas and main pancreatic duct. A 12-15 mm hemorrhagic “cauliflower” mass was also found which was oozing and friable. Biopsy was consistent with intraductal papillary mucinous neoplasm. The patient subsequently underwent a successful Whipple procedure. Surgical pathology returned showing intra-ampullary papillary tubular neoplasms (IAPN) with high grade dysplasia, and resection margins negative for neoplasm.
Discussion: With technological advancements in radiographic and endoscopic imaging, the incidence of IPMN has increased. CT fish mouth ampulla sign (continuous water attenuation from the pancreatic duct to the duodenal lumen) and endoscopic fish mouth ampulla (E-FMA) signs are highly specific for main duct and mixed IPMN. Our patient’s findings are unique in that her ERCP showed a hemorrhagic mass representing an unusual presentation of a common pancreatic lesion. Additionally, we aim to illustrate the importance of early endoscopic evaluation with endoscopy in patients with pancreatic changes on cross sectional imaging. The malignant potential for main duct IPMN is greater than for branch and mixed type IPMNs and therefore more commonly surgically resected.
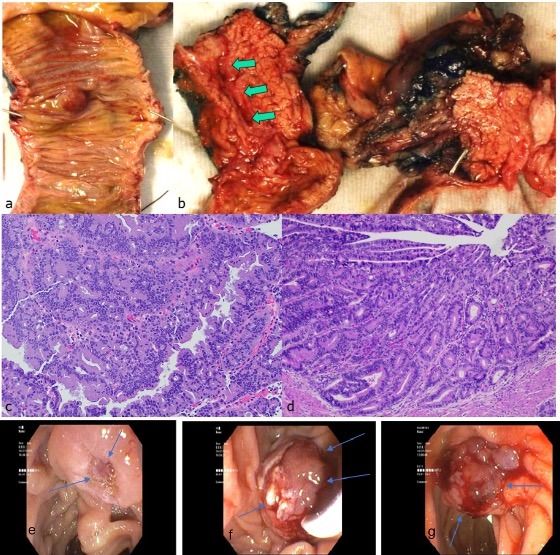
Figure: Figure 1: (a) The mass is extensively involving the ampulla of vater (seen from the duodenum) bulging out into the duodenal lumen; (b) Whipple specimen showing dilated pancreatic duct. Microscopically, both EUS aspiration biopsy (c, cell block) and the whipple specimen (d) show mucinous adenocarcinoma with identical tumor morphology. [c and d, Hematoxylin and Eosin stain, 40x magnification]. Subsequent ERCP demonstrating fish mouth ampulla (e), cauliflower mass with stent placement (f), hemorrhagic mass with friability (g).
Disclosures:
Harsh Patel indicated no relevant financial relationships.
Sarah Huang indicated no relevant financial relationships.
Dean Rizzi indicated no relevant financial relationships.
Navim Mobin indicated no relevant financial relationships.
Yani Zhao indicated no relevant financial relationships.
Shah Giashuddin indicated no relevant financial relationships.
Mukul Arya indicated no relevant financial relationships.
Harsh Patel, MD, MPH1, Sarah Huang, MD1, Dean Rizzi, MD2, Navim Mobin, MD1, Yani Zhao, MD3, Shah Giashuddin, MD4, Mukul Arya, MD5. A0074 - A Unique Endoscopic Presentation of Intraductal Papillary Mucinous Neoplasms (IPMN) Presenting as a Hemorrhagic Mass, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
