Back

Poster Session C - Monday Afternoon
Category: Biliary/Pancreas
C0059 - Missing the Viewing Angle on Obstructive Jaundice: Lemmel’s Syndrome
Monday, October 24, 2022
3:00 PM – 5:00 PM ET
Location: Crown Ballroom
Has Audio

Charles P. Cavalaris, MD
University of South Florida Morsani College of Medicine
Tampa, Florida
Presenting Author(s)
Charles P. Cavalaris, MD1, Bharat Ponnaganti, MD1, Shreya Narayanan, MD1, Brijesh Patel, MD2, Jason M. Colizzo, MD2
1University of South Florida Morsani College of Medicine, Tampa, FL; 2James A. Haley VA Hospital, Tampa, FL
Introduction: Lemmel’s syndrome (LS) is a rare form of obstructive jaundice that is often misdiagnosed. We report a case of elusive jaundice masquerading as DILI until endoscopy revealed the presence of a periampullary diverticulum.
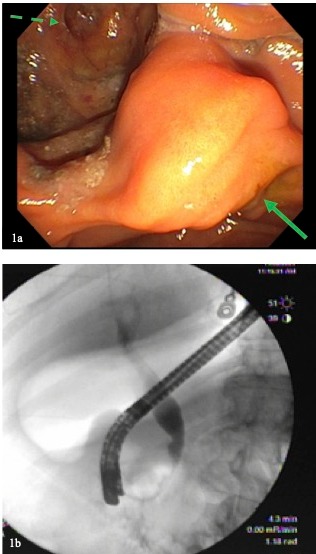
Case Description/Methods: A 79-year-old man presented with fatigue and pruritus. Medical history was notable for recent E. coli bacteremia treated with cefdinir. Upon presentation, vital signs were normal. Laboratory studies revealed total bilirubin 8.6 mg/dL, direct bilirubin 6.1 mg/dL, AST 106 U/L, ALT 236 U/L, alkaline phosphatase 854 U/L, and GGT 1120 U/L. CT of the abdomen/pelvis showed dilation of the pancreatic duct and intra/extrahepatic bile ducts. MRCP had similar findings but no biliary stones or masses. Dedicated CT of the pancreas was also negative for pancreatic or biliary lesions. EGD with EUS showed ductal dilation but was otherwise unremarkable. Liver biopsy revealed evidence of cholestasis. Steroid therapy was started for possible DILI however cholestasis continued to worsen and abdominal pain ensued. Repeat EGD with a duodenoscope revealed a patulous ampulla and large periampullary diverticulum (1a). ERCP was performed revealing no choledocholithiasis or stricture; however, an irregularity was found in the distal CBD due to compression from the diverticulum (1b). Cytology was obtained from the CBD irregularity which showed benign biliary epithelium. The diagnosis of LS was made and a 10Fr 7cm plastic biliary stent was placed. The patient’s bilirubin and alkaline phosphatase quickly improved from a peak of 17.8 mg/dL and 1036 U/L, respectively, to 8.5 mg/dL and 719 U/L within 24 hours of stent placement. Due to recurrent cholangitis requiring multiple ERCPs the patient is awaiting diverticulectomy and cholecystectomy for definitive management.
Discussion: LS is characterized by obstructive jaundice due to a periampullary diverticulum. In many patients the diagnosis can be challenging. In this case the presumption of DILI led to a delay in diagnosis. Only in the setting of persistent jaundice and worsening right upper quadrant abdominal pain was the possibility of LS entertained. In hindsight, the patient’s initial bacteremia was likely due to cholangitis due to LS. EGD with duodenoscope helped to confirm the diagnosis. Visualization of a periampullary diverticulum via duodenoscope is considered the gold-standard diagnostic modality for LS. Its use should be considered in cases where suspicion for LS is raised.
Disclosures:
Charles P. Cavalaris, MD1, Bharat Ponnaganti, MD1, Shreya Narayanan, MD1, Brijesh Patel, MD2, Jason M. Colizzo, MD2. C0059 - Missing the Viewing Angle on Obstructive Jaundice: Lemmel’s Syndrome, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1University of South Florida Morsani College of Medicine, Tampa, FL; 2James A. Haley VA Hospital, Tampa, FL
Introduction: Lemmel’s syndrome (LS) is a rare form of obstructive jaundice that is often misdiagnosed. We report a case of elusive jaundice masquerading as DILI until endoscopy revealed the presence of a periampullary diverticulum.
Case Description/Methods: A 79-year-old man presented with fatigue and pruritus. Medical history was notable for recent E. coli bacteremia treated with cefdinir. Upon presentation, vital signs were normal. Laboratory studies revealed total bilirubin 8.6 mg/dL, direct bilirubin 6.1 mg/dL, AST 106 U/L, ALT 236 U/L, alkaline phosphatase 854 U/L, and GGT 1120 U/L. CT of the abdomen/pelvis showed dilation of the pancreatic duct and intra/extrahepatic bile ducts. MRCP had similar findings but no biliary stones or masses. Dedicated CT of the pancreas was also negative for pancreatic or biliary lesions. EGD with EUS showed ductal dilation but was otherwise unremarkable. Liver biopsy revealed evidence of cholestasis. Steroid therapy was started for possible DILI however cholestasis continued to worsen and abdominal pain ensued. Repeat EGD with a duodenoscope revealed a patulous ampulla and large periampullary diverticulum (1a). ERCP was performed revealing no choledocholithiasis or stricture; however, an irregularity was found in the distal CBD due to compression from the diverticulum (1b). Cytology was obtained from the CBD irregularity which showed benign biliary epithelium. The diagnosis of LS was made and a 10Fr 7cm plastic biliary stent was placed. The patient’s bilirubin and alkaline phosphatase quickly improved from a peak of 17.8 mg/dL and 1036 U/L, respectively, to 8.5 mg/dL and 719 U/L within 24 hours of stent placement. Due to recurrent cholangitis requiring multiple ERCPs the patient is awaiting diverticulectomy and cholecystectomy for definitive management.
Discussion: LS is characterized by obstructive jaundice due to a periampullary diverticulum. In many patients the diagnosis can be challenging. In this case the presumption of DILI led to a delay in diagnosis. Only in the setting of persistent jaundice and worsening right upper quadrant abdominal pain was the possibility of LS entertained. In hindsight, the patient’s initial bacteremia was likely due to cholangitis due to LS. EGD with duodenoscope helped to confirm the diagnosis. Visualization of a periampullary diverticulum via duodenoscope is considered the gold-standard diagnostic modality for LS. Its use should be considered in cases where suspicion for LS is raised.
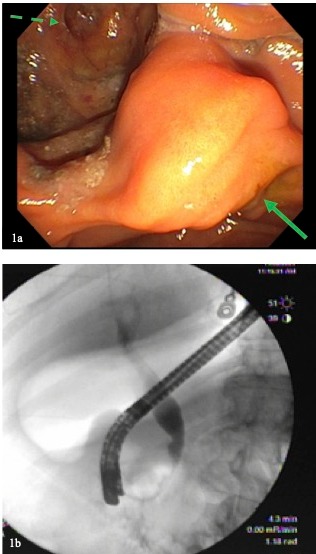
Figure: (1a) Periampullary diverticulum, with solid arrow demarcating the papilla and dashed arrow revealing the large periampullary diverticulum containing smaller internal diverticuli. (1b) ERCP with cholangiogram showing external compression of CBD by the periampullary diverticulum with upstream ductal dilation.
Disclosures:
Charles Cavalaris indicated no relevant financial relationships.
Bharat Ponnaganti indicated no relevant financial relationships.
Shreya Narayanan indicated no relevant financial relationships.
Brijesh Patel indicated no relevant financial relationships.
Jason Colizzo indicated no relevant financial relationships.
Charles P. Cavalaris, MD1, Bharat Ponnaganti, MD1, Shreya Narayanan, MD1, Brijesh Patel, MD2, Jason M. Colizzo, MD2. C0059 - Missing the Viewing Angle on Obstructive Jaundice: Lemmel’s Syndrome, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
