Back

Poster Session D - Tuesday Morning
Category: Endoscopy Video Forum
D0186 - Endoscopic Full-Thickness Resection of Gastric Ulceration with Persistent Low-Grade Dysplasia Using the Full-Thickness Resection Device
Tuesday, October 25, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom
Has Audio
.jpg)
Natalie Wilson, MD
University of Minnesota
Minneapolis, MN
Presenting Author(s)
Natalie Wilson, MD1, Nicholas McDonald, MD1, Mohamed Abdallah, MD2, Mohammad Bilal, MD3
1University of Minnesota, Minneapolis, MN; 2University of Minnesota Medical Center, Minneapolis, MN; 3University of Minnesota, Minneapolis VA Medical Center, Minneapolis, MN
Introduction: Endoscopic mucosal resection (EMR) and endoscopic submucosal dissection (ESD) are well-established treatment methods for resection of precancerous gastric lesions and early gastric cancers. Ulcerated or scarred gastric lesions are challenging to resect with EMR or ESD due to submucosal fibrosis and scarring, and hence, carry an increased risk for perforation.
Endoscopic full-thickness resection (EFTR) using the full-thickness resection device (FTRD) is rapidly gaining popularity for the treatment of upper gastrointestinal tract lesions. While it has been shown to be a safe and effective treatment modality for colorectal lesions not amenable to conventional resection methods, data regarding its use in the upper GI tract is evolving.
Here, we describe a patient with an ulcerated gastric lesion with persistent low-grade dysplasia who underwent successful resection of the lesion using the FTRD.
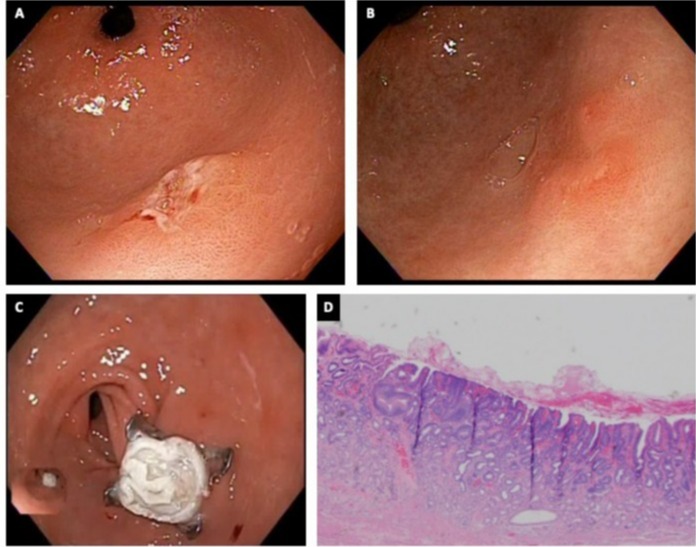
Case Description/Methods: A 75-year-old man with a history of diffuse gastric intestinal metaplasia was found to have a 1 cm ulcer in the gastric antrum (Figure 1A). Biopsies of the ulcer demonstrated low-grade dysplasia, while surrounding biopsies showed incomplete gastric intestinal metaplasia. He was started on a proton pump inhibitor with plan for repeat endoscopy for surveillance.
Subsequent upper endoscopy 12 and 24 months later showed partial healing of the gastric ulcer (Figure 1B), however, biopsies showed persistent low-grade dysplasia. After a multidisciplinary discussion, the decision was made to pursue EFTR of the ulcerated lesion.
An upper endoscopy was performed and the borders of the lesion were marked circumferentially with a marking probe. The FTRD was mounted on a modified therapeutic upper endoscope and the lesion was resected. The resection site was examined and demonstrated appropriate positioning of the clip and no evidence of bleeding (Figure 1C). Given the proximity of the lesion to the pylorus, the endoscope was advanced to the duodenum documenting luminal patency.
The patient tolerated the procedure well and was discharged the same day. No adverse events were experienced within four weeks of the procedure. The final pathology report of the lesion confirmed focal low-grade dysplasia (Figure 1D) with negative resection margins (R0).
Discussion: EFTR using the FTRD device can offer a safe and effective approach to treat ulcerated or scarred gastric lesions that are not typically amenable to conventional endoscopic resection techniques.
Disclosures:
Natalie Wilson, MD1, Nicholas McDonald, MD1, Mohamed Abdallah, MD2, Mohammad Bilal, MD3. D0186 - Endoscopic Full-Thickness Resection of Gastric Ulceration with Persistent Low-Grade Dysplasia Using the Full-Thickness Resection Device, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1University of Minnesota, Minneapolis, MN; 2University of Minnesota Medical Center, Minneapolis, MN; 3University of Minnesota, Minneapolis VA Medical Center, Minneapolis, MN
Introduction: Endoscopic mucosal resection (EMR) and endoscopic submucosal dissection (ESD) are well-established treatment methods for resection of precancerous gastric lesions and early gastric cancers. Ulcerated or scarred gastric lesions are challenging to resect with EMR or ESD due to submucosal fibrosis and scarring, and hence, carry an increased risk for perforation.
Endoscopic full-thickness resection (EFTR) using the full-thickness resection device (FTRD) is rapidly gaining popularity for the treatment of upper gastrointestinal tract lesions. While it has been shown to be a safe and effective treatment modality for colorectal lesions not amenable to conventional resection methods, data regarding its use in the upper GI tract is evolving.
Here, we describe a patient with an ulcerated gastric lesion with persistent low-grade dysplasia who underwent successful resection of the lesion using the FTRD.
Case Description/Methods: A 75-year-old man with a history of diffuse gastric intestinal metaplasia was found to have a 1 cm ulcer in the gastric antrum (Figure 1A). Biopsies of the ulcer demonstrated low-grade dysplasia, while surrounding biopsies showed incomplete gastric intestinal metaplasia. He was started on a proton pump inhibitor with plan for repeat endoscopy for surveillance.
Subsequent upper endoscopy 12 and 24 months later showed partial healing of the gastric ulcer (Figure 1B), however, biopsies showed persistent low-grade dysplasia. After a multidisciplinary discussion, the decision was made to pursue EFTR of the ulcerated lesion.
An upper endoscopy was performed and the borders of the lesion were marked circumferentially with a marking probe. The FTRD was mounted on a modified therapeutic upper endoscope and the lesion was resected. The resection site was examined and demonstrated appropriate positioning of the clip and no evidence of bleeding (Figure 1C). Given the proximity of the lesion to the pylorus, the endoscope was advanced to the duodenum documenting luminal patency.
The patient tolerated the procedure well and was discharged the same day. No adverse events were experienced within four weeks of the procedure. The final pathology report of the lesion confirmed focal low-grade dysplasia (Figure 1D) with negative resection margins (R0).
Discussion: EFTR using the FTRD device can offer a safe and effective approach to treat ulcerated or scarred gastric lesions that are not typically amenable to conventional endoscopic resection techniques.
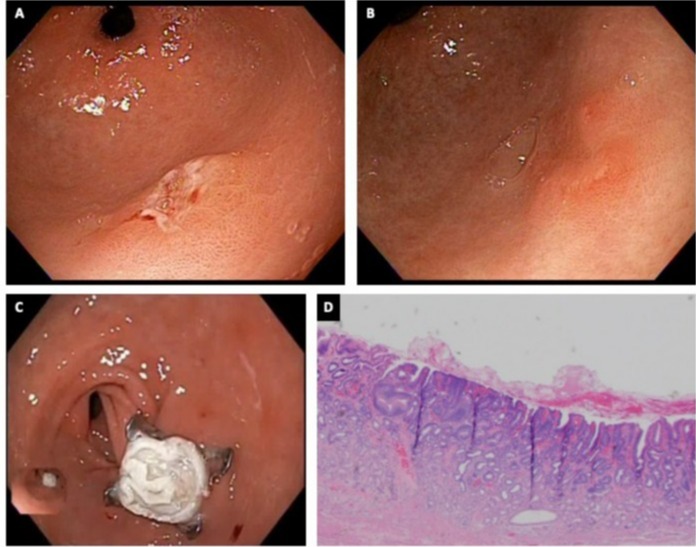
Figure: Figure 1. A) Initial upper endoscopy with antral gastric ulcer. B) Subsequent upper endoscopy showing partial healing of the gastric ulcer. C) Endoscopic view of the resection site with overlying clip after EFTR. D) Pathology of resected lesion demonstrating focal low-grade dysplasia.
Disclosures:
Natalie Wilson indicated no relevant financial relationships.
Nicholas McDonald indicated no relevant financial relationships.
Mohamed Abdallah indicated no relevant financial relationships.
Mohammad Bilal indicated no relevant financial relationships.
Natalie Wilson, MD1, Nicholas McDonald, MD1, Mohamed Abdallah, MD2, Mohammad Bilal, MD3. D0186 - Endoscopic Full-Thickness Resection of Gastric Ulceration with Persistent Low-Grade Dysplasia Using the Full-Thickness Resection Device, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
