Back

Poster Session D - Tuesday Morning
Category: Colon
D0124 - Strongyloides-Associated Eosinophilic Colitis: Implications for Managing Renal Transplant Patients
Tuesday, October 25, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom
Has Audio

Eitan Scheinthal, DO
CMSRU/Cooper University Hospital
Camden, NJ
Presenting Author(s)
Eitan Scheinthal, DO1, Pilin Francis, DO2, Krysta Contino, MD1, Hadi Shojaei, MD1
1CMSRU/Cooper University Hospital, Camden, NJ; 2Cooper University Hospital, Camden, NJ
Introduction: Strongyloides stercoralis is a parasitic intestinal nematode that is often asymptomatic but can cause life threatening hyperinfection syndrome (HIS) and disseminated disease (DD). Solid organ transplant patients require careful evaluation. Diagnostic challenges may allow patients to proceed to transplantation, increasing risk for HIS. These infections prove difficult to identify and treat, with high mortality rates.
Case Description/Methods: A 57-year-old man with CKD on peritoneal dialysis and chronic pancreatitis complicated by pseudocyst formation with cyst gastrostomy undergoing renal transplant evaluation presented for chronic abdominal pain, daily diarrhea, postprandial dyspepsia and 35lb weight loss over two years. He required multiple hospitalizations and endoscopic evaluation without clear diagnosis. He was clinically stable on pancrelipase for presumed exocrine pancreatic insufficiency. Labs showed lipase 41, triglycerides 173, IgG4 32, WBC 9.6 with eosinophils 100/µL, Iron 79. Colonoscopy showed granular transverse colonic mucosa that was biopsied. Pathology showed intraepithelial and lamina propria eosinophils. Immunohistochemical staining for CD117 did not show increased mast cells. Follow up tryptase was 12.9 and eosinophils 660/µL. IgA 147, IgG 2253 and IgM 50. IgE was not assessed. Stool studies and allergy skin testing were negative. Strongyloides IgG antibody returned positive. He was treated with Ivermectin 15mg (200mcg/kg/day) induction for two days followed by Ivermectin 15mg for two days, 14 days later. Subsequent laboratory testing confirmed resolution with improvement in peripheral eosinophilia and with resolution of his diarrhea.
Discussion: Strongyloides infection is well described in solid organ transplant patients. Larvae introduce enteric bacteria or fungi into the blood causing electrolyte disturbances, colonic ulceration, alveolar hemorrhage, severe sepsis and death. Morbidity and mortality, reaches 50% for HIS and 70% for DD. Diagnosis requires larvae identification but false negatives are high. Duodenal aspirates have better sensitivity at 76%. Serologic testing cannot distinguish between prior or active infection. A gelatin particle indirect agglutination test may be more reliable. First line treatment with Ivermectin induction with later treatment effectively eradicates organisms with cure rates between 94-100%. In our case, early detection may have prevented HIS and highlights the significance of early detection, particularly in pre-transplant patients.
Disclosures:
Eitan Scheinthal, DO1, Pilin Francis, DO2, Krysta Contino, MD1, Hadi Shojaei, MD1. D0124 - Strongyloides-Associated Eosinophilic Colitis: Implications for Managing Renal Transplant Patients, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1CMSRU/Cooper University Hospital, Camden, NJ; 2Cooper University Hospital, Camden, NJ
Introduction: Strongyloides stercoralis is a parasitic intestinal nematode that is often asymptomatic but can cause life threatening hyperinfection syndrome (HIS) and disseminated disease (DD). Solid organ transplant patients require careful evaluation. Diagnostic challenges may allow patients to proceed to transplantation, increasing risk for HIS. These infections prove difficult to identify and treat, with high mortality rates.
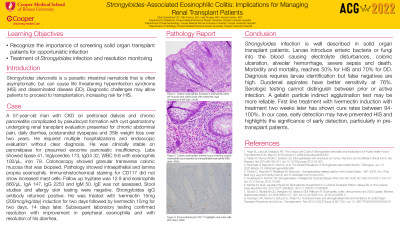
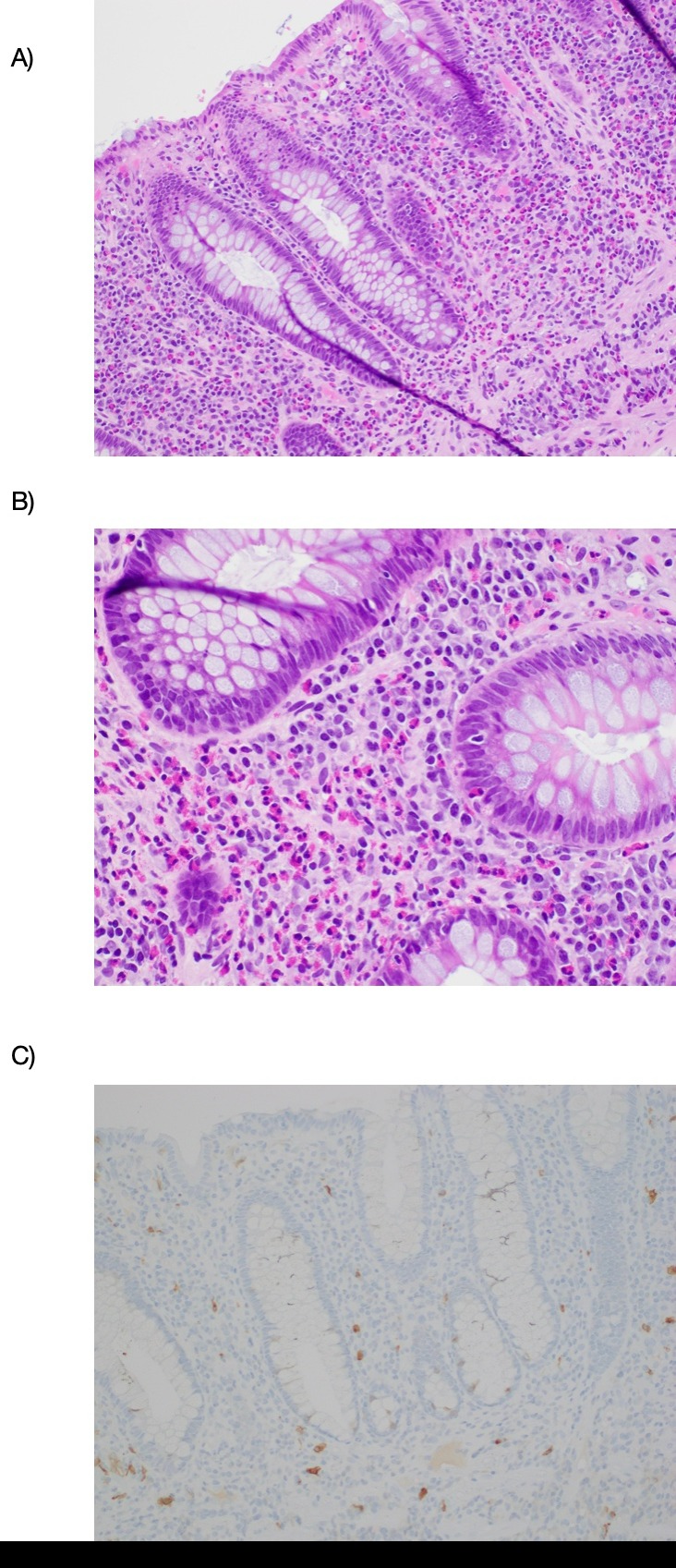
Case Description/Methods: A 57-year-old man with CKD on peritoneal dialysis and chronic pancreatitis complicated by pseudocyst formation with cyst gastrostomy undergoing renal transplant evaluation presented for chronic abdominal pain, daily diarrhea, postprandial dyspepsia and 35lb weight loss over two years. He required multiple hospitalizations and endoscopic evaluation without clear diagnosis. He was clinically stable on pancrelipase for presumed exocrine pancreatic insufficiency. Labs showed lipase 41, triglycerides 173, IgG4 32, WBC 9.6 with eosinophils 100/µL, Iron 79. Colonoscopy showed granular transverse colonic mucosa that was biopsied. Pathology showed intraepithelial and lamina propria eosinophils. Immunohistochemical staining for CD117 did not show increased mast cells. Follow up tryptase was 12.9 and eosinophils 660/µL. IgA 147, IgG 2253 and IgM 50. IgE was not assessed. Stool studies and allergy skin testing were negative. Strongyloides IgG antibody returned positive. He was treated with Ivermectin 15mg (200mcg/kg/day) induction for two days followed by Ivermectin 15mg for two days, 14 days later. Subsequent laboratory testing confirmed resolution with improvement in peripheral eosinophilia and with resolution of his diarrhea.
Discussion: Strongyloides infection is well described in solid organ transplant patients. Larvae introduce enteric bacteria or fungi into the blood causing electrolyte disturbances, colonic ulceration, alveolar hemorrhage, severe sepsis and death. Morbidity and mortality, reaches 50% for HIS and 70% for DD. Diagnosis requires larvae identification but false negatives are high. Duodenal aspirates have better sensitivity at 76%. Serologic testing cannot distinguish between prior or active infection. A gelatin particle indirect agglutination test may be more reliable. First line treatment with Ivermectin induction with later treatment effectively eradicates organisms with cure rates between 94-100%. In our case, early detection may have prevented HIS and highlights the significance of early detection, particularly in pre-transplant patients.
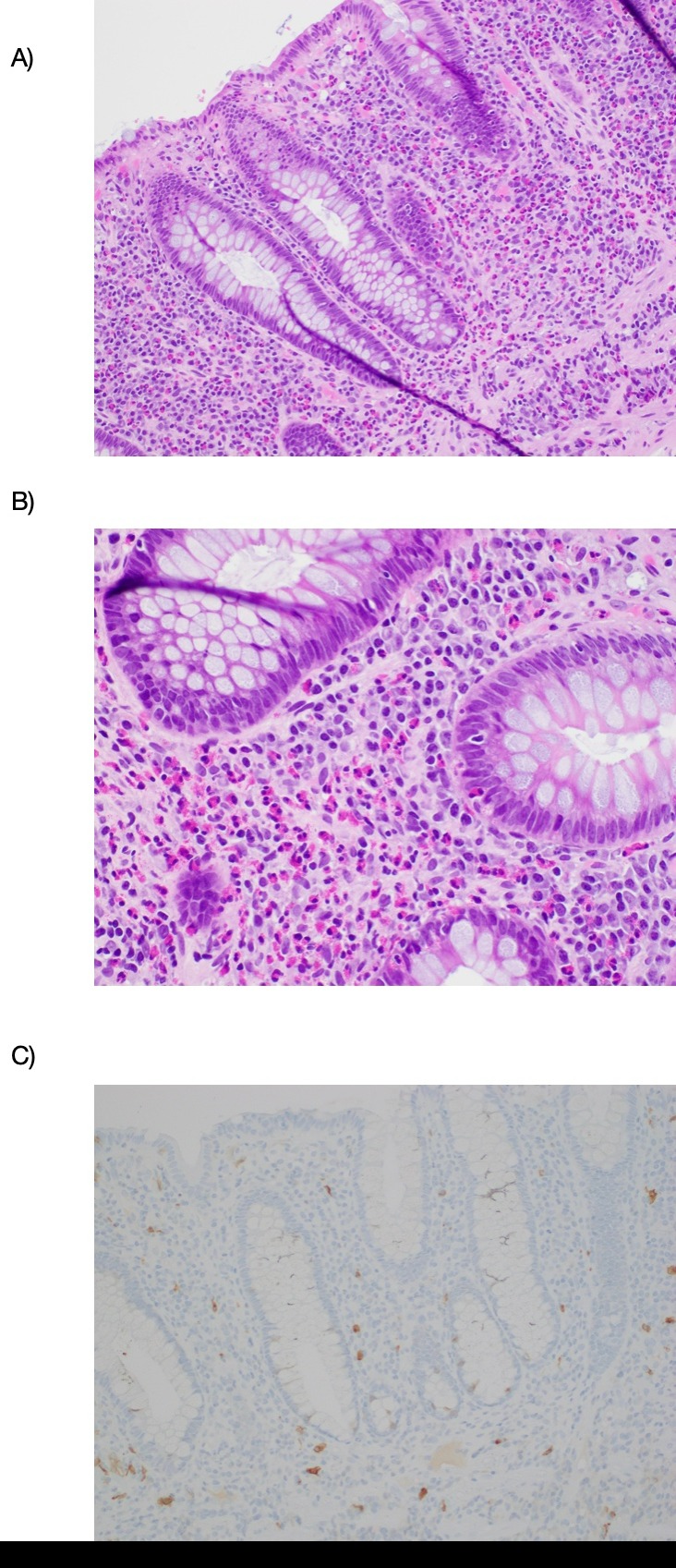
Figure: Figure 1. Colonic eosinophilia
(A) Increase in eosinophils within the mucosa and submucosa with preserved crypt architecture (H&E stain; 200X)
(B) Intense focus of lamina propria eosinophilia accompanied by intraepithelial eosinophils (H&E stain; 400x)
(C) Immunostaining for CD117 highlights rare mast cells (IHC stain; 200X)
(A) Increase in eosinophils within the mucosa and submucosa with preserved crypt architecture (H&E stain; 200X)
(B) Intense focus of lamina propria eosinophilia accompanied by intraepithelial eosinophils (H&E stain; 400x)
(C) Immunostaining for CD117 highlights rare mast cells (IHC stain; 200X)
Disclosures:
Eitan Scheinthal indicated no relevant financial relationships.
Pilin Francis indicated no relevant financial relationships.
Krysta Contino indicated no relevant financial relationships.
Hadi Shojaei indicated no relevant financial relationships.
Eitan Scheinthal, DO1, Pilin Francis, DO2, Krysta Contino, MD1, Hadi Shojaei, MD1. D0124 - Strongyloides-Associated Eosinophilic Colitis: Implications for Managing Renal Transplant Patients, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
