Back

Poster Session D - Tuesday Morning
Category: Esophagus
D0194 - Dupilumab Improves Clinical, Symptomatic, Histologic, and Endoscopic Aspects of EoE, Regardless of Prior Swallowed Topical Steroid Use
Tuesday, October 25, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom
Has Audio
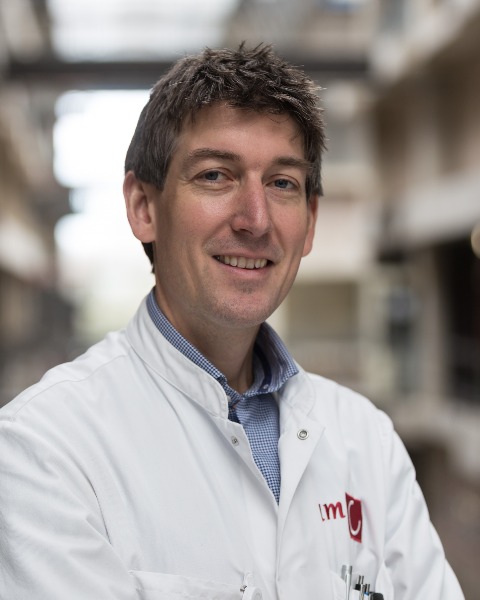
Albert Bredenoord, MD, PhD
Amsterdam University Medical Center
Amsterdam, Utrecht, Netherlands
Presenting Author(s)
Albert Bredenoord, MD, PhD1, Evan Dellon, MD, MPH2, Alfredo Lucendo, MD3, Margaret Collins, MD, PhD4, Xian Sun, PhD5, Kiran Patel, PhD6, Bethany Beazley, PhD5, Arsalan Shabbir, PhD5
1Amsterdam University Medical Center, Amsterdam, Utrecht, Netherlands; 2University of North Carolina School of Medicine, Chapel Hill, NC; 3Hospital General de Tomelloso, Tomelloso, Madrid, Spain; 4Cincinnati Children’s Hospital Medical Center and University of Cincinnati College of Medicine, Cincinnati, OH; 5Regeneron Pharmaceuticals, Tarrytown, NY; 6Sanofi, Tarrytown, NY
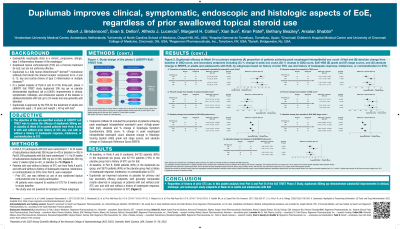
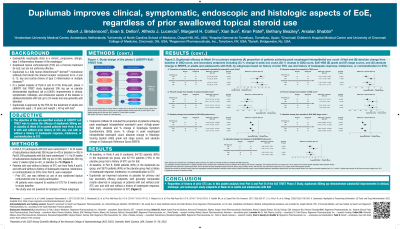
Introduction: Swallowed topical corticosteroids (STC) are a first-line treatment for eosinophilic esophagitis (EoE) but are not uniformly effective. Dupilumab, a fully human monoclonal antibody, blocks the shared receptor component for IL-4/IL-13, key and central drivers of type 2 inflammation. In Parts A and B of the phase 3 LIBERTY-EoE-TREET (NCT03633617) study, weekly dupilumab 300mg improved clinical, symptomatic, histologic, and endoscopic aspects of EoE and was generally well tolerated in adult and adolescent patients with EoE. The objective of this analysis was to assess the efficacy of weekly dupilumab 300mg vs placebo at Week 24 in patients from Part B with and without prior STC use history for EoE.
Methods: Patients who received STCs for EoE ≤8 weeks prior to baseline were excluded from the study. Endpoints at Week 24 were: proportion achieving peak eosinophil count (PEC) ≤6/high-power field (hpf); absolute and % change in Dysphagia Symptom Questionnaire (DSQ) score; % change in PEC; absolute change in Histologic Scoring System (HSS) grade and stage scores and Endoscopic Reference Score (EREFS).
Results: 55/80 (69%) and 56/79 (71%) of dupilumab- and placebo-treated patients had STC use history; 38/80 (48%) and 39/79 (49%) of dupilumab- and placebo-treated patients had inadequate response/intolerance/contraindication to STCs. For patients treated with dupilumab qw vs placebo PEC≤6/hpf was achieved by 63.6% vs 5.4% of patients with, and 48.0% vs 8.7% without prior STC use. Difference vs placebo (95% CI) for patients with/without prior STC use: absolute change in DSQ −11.63 (−17.64,−5.62)/−6.79 (−15.78,2.20); % change in PEC −86.97 (−116.38,−57.57)/−91.23 (−124.23,−58.24); absolute change in EoE-HSS grade −0.73 (−0.86,−0.60)/−0.58 (−0.80,−0.35) and stage −0.74 (−0.87,−0.62)/−0.54 (−0.75,−0.33); absolute change in EREFS −4.2 (−5.31,−3.18)/−2.7 (−4.58,−0.86); % change in DSQ −49.3 (−72.3, −26.2)/−20.8 (−58.3,16.7). Dupilumab was generally well tolerated in the intent-to-treat population; the most common TEAEs for dupilumab/placebo were injection-site reactions (37.5/33.3%).
Discussion: In Part B of this phase 3 study, dupilumab improved clinical, symptomatic, histologic, and endoscopic aspects of EoE regardless of STC use history.
Disclosures:
Albert Bredenoord, MD, PhD1, Evan Dellon, MD, MPH2, Alfredo Lucendo, MD3, Margaret Collins, MD, PhD4, Xian Sun, PhD5, Kiran Patel, PhD6, Bethany Beazley, PhD5, Arsalan Shabbir, PhD5. D0194 - Dupilumab Improves Clinical, Symptomatic, Histologic, and Endoscopic Aspects of EoE, Regardless of Prior Swallowed Topical Steroid Use, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1Amsterdam University Medical Center, Amsterdam, Utrecht, Netherlands; 2University of North Carolina School of Medicine, Chapel Hill, NC; 3Hospital General de Tomelloso, Tomelloso, Madrid, Spain; 4Cincinnati Children’s Hospital Medical Center and University of Cincinnati College of Medicine, Cincinnati, OH; 5Regeneron Pharmaceuticals, Tarrytown, NY; 6Sanofi, Tarrytown, NY
Introduction: Swallowed topical corticosteroids (STC) are a first-line treatment for eosinophilic esophagitis (EoE) but are not uniformly effective. Dupilumab, a fully human monoclonal antibody, blocks the shared receptor component for IL-4/IL-13, key and central drivers of type 2 inflammation. In Parts A and B of the phase 3 LIBERTY-EoE-TREET (NCT03633617) study, weekly dupilumab 300mg improved clinical, symptomatic, histologic, and endoscopic aspects of EoE and was generally well tolerated in adult and adolescent patients with EoE. The objective of this analysis was to assess the efficacy of weekly dupilumab 300mg vs placebo at Week 24 in patients from Part B with and without prior STC use history for EoE.
Methods: Patients who received STCs for EoE ≤8 weeks prior to baseline were excluded from the study. Endpoints at Week 24 were: proportion achieving peak eosinophil count (PEC) ≤6/high-power field (hpf); absolute and % change in Dysphagia Symptom Questionnaire (DSQ) score; % change in PEC; absolute change in Histologic Scoring System (HSS) grade and stage scores and Endoscopic Reference Score (EREFS).
Results: 55/80 (69%) and 56/79 (71%) of dupilumab- and placebo-treated patients had STC use history; 38/80 (48%) and 39/79 (49%) of dupilumab- and placebo-treated patients had inadequate response/intolerance/contraindication to STCs. For patients treated with dupilumab qw vs placebo PEC≤6/hpf was achieved by 63.6% vs 5.4% of patients with, and 48.0% vs 8.7% without prior STC use. Difference vs placebo (95% CI) for patients with/without prior STC use: absolute change in DSQ −11.63 (−17.64,−5.62)/−6.79 (−15.78,2.20); % change in PEC −86.97 (−116.38,−57.57)/−91.23 (−124.23,−58.24); absolute change in EoE-HSS grade −0.73 (−0.86,−0.60)/−0.58 (−0.80,−0.35) and stage −0.74 (−0.87,−0.62)/−0.54 (−0.75,−0.33); absolute change in EREFS −4.2 (−5.31,−3.18)/−2.7 (−4.58,−0.86); % change in DSQ −49.3 (−72.3, −26.2)/−20.8 (−58.3,16.7). Dupilumab was generally well tolerated in the intent-to-treat population; the most common TEAEs for dupilumab/placebo were injection-site reactions (37.5/33.3%).
Discussion: In Part B of this phase 3 study, dupilumab improved clinical, symptomatic, histologic, and endoscopic aspects of EoE regardless of STC use history.
Disclosures:
Albert Bredenoord: Arena Pharmaceuticals – Consultant. AstraZeneca – Consultant. Bayer – Stock Options. Calypso Biotech – Consultant. Dr Falk – Consultant. EsoCap – Consultant. Gossamer Bio – Consultant. Laborie – Consultant. Medtronic – Consultant. Nutricia – Stock Options. RB Pharma – Consultant. Regeneron Pharmaceuticals, Inc. – Consultant. Robarts Clinical Trials – Consultant. SST – Grant/Research Support. SST – Stock Options.
Evan Dellon: Abbott – Consultant. Abbvie – Consultant. Adare Pharma Solutions – Consultant, Grant/Research Support. Aimmune Therapeutics – Consultant. Allakos – Consultant, Grant/Research Support, Educational grant. Amgen – Consultant. Arena Pharmaceuticals – Consultant, Grant/Research Support. AstraZeneca – Consultant, Grant/Research Support. Banner Pharmaceuticals – Grant/Research Support. Biorasi – Consultant. Calypso Biotech – Consultant. Eli Lilly – Consultant. EsoCap – Consultant. Gossamer Bio – Consultant. GSK – Consultant, Grant/Research Support. Holoclara – Grant/Research Support. Invea Therapeutics – Consultant. Landos Biopharma – Consultant. Lucid Diagnostics – Consultant. LucidDX – Consultant. Meritage Pharma – Consultant, Grant/Research Support. Miraca Life Sciences – Consultant, Grant/Research Support. Morphic Therapeutic – Consultant. Nutricia – Consultant, Grant/Research Support. Parexel/Calyx – Consultant. Phathom Pharmaceuticals – Consultant. Receptos/BMS – Consultant, Grant/Research Support. Regeneron Pharmaceuticals, Inc. – Consultant, Grant/Research Support. Revolo Bio – Consultant. Robarts Clinical Trials/Alimentiv – Consultant. Salix Pharmaceuticals – Consultant. Sanofi – Consultant. Shire/Takeda – Consultant, Grant/Research Support. Target RWE/Ellodi Pharmaceuticals – Consultant.
Alfredo Lucendo: Dr. Falk Pharma – Consultant. EsoCap – Consultant. Regeneron Pharmaceuticals, Inc – Grant/Research Support.
Margaret Collins: Alimentiv – Consultant. Allakos – Consultant. Arena Pharmaceuticals – Consultant. AstraZeneca – Consultant. AstraZeneca – Grant/Research Support. Calypso Biotech – Consultant. EsoCap – Consultant. GSK – Consultant. Receptos/Celgene/BMS – Consultant. Receptos/Celgene/BMS – Grant/Research Support. Regeneron Pharmaceuticals, Inc. – Consultant. Regeneron Pharmaceuticals, Inc. – Grant/Research Support. Shire a Takeda company – Consultant. Shire a Takeda company – Grant/Research Support.
Xian Sun: Regeneron Pharmaceuticals, Inc. – Employee, Stock Options.
Kiran Patel: Sanofi – Employee, Stock Options.
Bethany Beazley: Regeneron Pharmaceuticals, Inc. – Employee, Stock Options.
Arsalan Shabbir: Regeneron Pharmaceuticals, Inc. – Employee, Stock Options.
Albert Bredenoord, MD, PhD1, Evan Dellon, MD, MPH2, Alfredo Lucendo, MD3, Margaret Collins, MD, PhD4, Xian Sun, PhD5, Kiran Patel, PhD6, Bethany Beazley, PhD5, Arsalan Shabbir, PhD5. D0194 - Dupilumab Improves Clinical, Symptomatic, Histologic, and Endoscopic Aspects of EoE, Regardless of Prior Swallowed Topical Steroid Use, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
