Back

Poster Session A - Sunday Afternoon
Category: Interventional Endoscopy
A0444 - Endoscopic Management of Dumping Syndrome in a Roux-en-Y Gastric Bypass (RYGB) Patient With Transoral Outlet Reduction and Remnant Stomach Access With Lumen Apposing Metal Stent
Sunday, October 23, 2022
5:00 PM – 7:00 PM ET
Location: Crown Ballroom
Has Audio
- KK
Ki-Yoon Kim, MD
Scripps
San Diego, CA
Presenting Author(s)
Ki-Yoon Kim, MD1, Franklin Tsai, MD2, Walter Coyle, MD2, Matthew J. Skinner, MD2
1Scripps, San Diego, CA; 2Scripps Green-Scripps Clinic, La Jolla, CA
Introduction: Dumping syndrome is a possible complication of RYGB. Treatment has been limited to dietary changes, medications, surgical reversal, and enteral nutrition. Recently, transoral gastric outlet reduction (TORe) and lumen apposing metal stent (LAMS) placement to access the remnant stomach have shown promising results. We report a patient with severe dumping syndrome who had significant improvement after both TORe and LAMS placement.
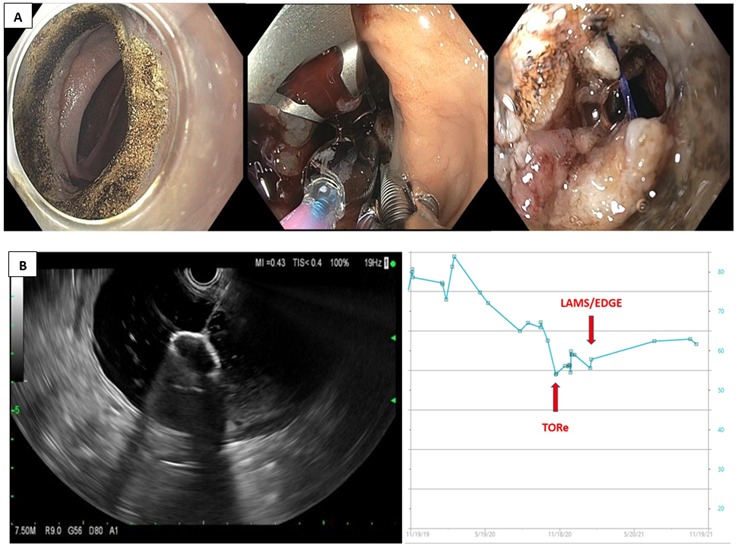
Case Description/Methods: 68 year old man underwent RYGB and presented with over 100 lbs weight loss, weakness, recurrent syncope, tachycardia, and persistent hypoglycemia. Initial Sigstad's score was 27. He had tachycardia of 105, BMI of 16.6, and cachexia resulting in non-ambulatory status. Labs showed potassium 3.2, bicarbonate 36, glucose 41, total protein 4.8, albumin 2.0, and prealbumin 7. Modified glucose tolerance test was positive. Exogenous insulin use, adrenal insufficiency, and insulinoma were ruled out. Despite behavioral modification, acarbose, and guar gum, he had persistent symptoms and became TPN dependent. He underwent TORe (Figure 1A), which improved Sigstad's score from 27 to 10 with 10 lbs weight regain in 2 months. Incidentally, patient developed choledocholithiasis and required LAMS placement for transgastric ERCP. After successful ERCP, the LAMS was intentionally left in place to allow access of food to the remnant stomach. In 8 months, Sigstad's score improved additionally from 10 to 5 and the weight increased additionally by 11 lbs (Figure 1B). After both procedures, he was ambulatory, on normal diet, and able to stop TPN. BMI improved to 20.1. Labs became normal.
Discussion: Dumping syndrome occurs as a result of rapid transit of hyperosmolar foods and carbohydrates in small intestine. This causes early and late dumping syndrome due to rapid fluid shift and hyperinsulinemic response, resulting in hypotension, tachycardia, and hypoglycemia. Sigstad's score above 7 suggests dumping syndrome. Modified glucose test confirms the diagnosis. Vargas et al reported 150 RYGB patients with severe dumping syndrome refractory to behavioral/medical treatment and underwent TORe. Sigstad's score improved from a mean of 17 to 2.6 (P=0.0001). The authors also consider LAMS placement to access remnant gastric stomach as another viable option and await prospective study results.
In conclusion, RYGB patients with severe dumping syndrome refractory to medical and behavioral therapy can be treated with TORe and LAMS placement to access the remnant stomach.
Disclosures:
Ki-Yoon Kim, MD1, Franklin Tsai, MD2, Walter Coyle, MD2, Matthew J. Skinner, MD2. A0444 - Endoscopic Management of Dumping Syndrome in a Roux-en-Y Gastric Bypass (RYGB) Patient With Transoral Outlet Reduction and Remnant Stomach Access With Lumen Apposing Metal Stent, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1Scripps, San Diego, CA; 2Scripps Green-Scripps Clinic, La Jolla, CA
Introduction: Dumping syndrome is a possible complication of RYGB. Treatment has been limited to dietary changes, medications, surgical reversal, and enteral nutrition. Recently, transoral gastric outlet reduction (TORe) and lumen apposing metal stent (LAMS) placement to access the remnant stomach have shown promising results. We report a patient with severe dumping syndrome who had significant improvement after both TORe and LAMS placement.
Case Description/Methods: 68 year old man underwent RYGB and presented with over 100 lbs weight loss, weakness, recurrent syncope, tachycardia, and persistent hypoglycemia. Initial Sigstad's score was 27. He had tachycardia of 105, BMI of 16.6, and cachexia resulting in non-ambulatory status. Labs showed potassium 3.2, bicarbonate 36, glucose 41, total protein 4.8, albumin 2.0, and prealbumin 7. Modified glucose tolerance test was positive. Exogenous insulin use, adrenal insufficiency, and insulinoma were ruled out. Despite behavioral modification, acarbose, and guar gum, he had persistent symptoms and became TPN dependent. He underwent TORe (Figure 1A), which improved Sigstad's score from 27 to 10 with 10 lbs weight regain in 2 months. Incidentally, patient developed choledocholithiasis and required LAMS placement for transgastric ERCP. After successful ERCP, the LAMS was intentionally left in place to allow access of food to the remnant stomach. In 8 months, Sigstad's score improved additionally from 10 to 5 and the weight increased additionally by 11 lbs (Figure 1B). After both procedures, he was ambulatory, on normal diet, and able to stop TPN. BMI improved to 20.1. Labs became normal.
Discussion: Dumping syndrome occurs as a result of rapid transit of hyperosmolar foods and carbohydrates in small intestine. This causes early and late dumping syndrome due to rapid fluid shift and hyperinsulinemic response, resulting in hypotension, tachycardia, and hypoglycemia. Sigstad's score above 7 suggests dumping syndrome. Modified glucose test confirms the diagnosis. Vargas et al reported 150 RYGB patients with severe dumping syndrome refractory to behavioral/medical treatment and underwent TORe. Sigstad's score improved from a mean of 17 to 2.6 (P=0.0001). The authors also consider LAMS placement to access remnant gastric stomach as another viable option and await prospective study results.
In conclusion, RYGB patients with severe dumping syndrome refractory to medical and behavioral therapy can be treated with TORe and LAMS placement to access the remnant stomach.
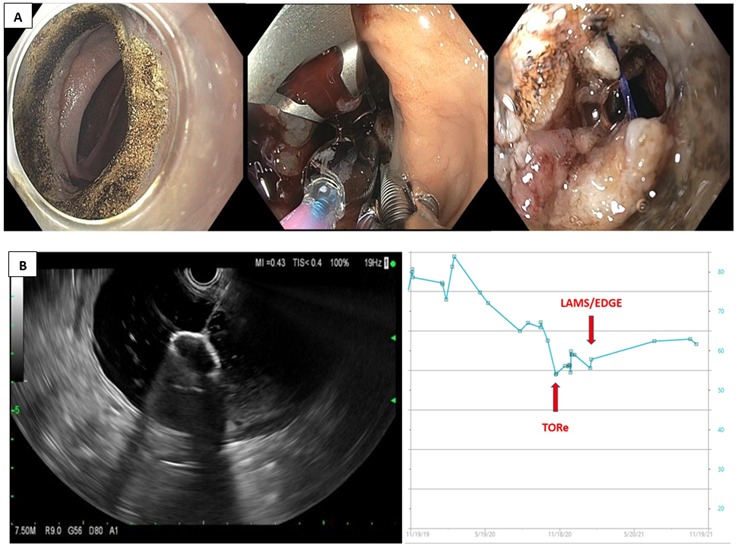
Figure: Figure 1A. Endoscopic Images of Transoral Gastric Outlet Revision with APC of the gastrojejunal anastomsis followed by purse string full thickness suturing over a 10 mm CRE balloon.
Figure 1B. EUS image of demonstrating distal phalange deployment of LAMS into the remnant stomach for EUS guided transgastric ERCP. B. Weight chart demonstrating weight loss after RYGB and regain with TORe and LAMS placement.
Figure 1B. EUS image of demonstrating distal phalange deployment of LAMS into the remnant stomach for EUS guided transgastric ERCP. B. Weight chart demonstrating weight loss after RYGB and regain with TORe and LAMS placement.
Disclosures:
Ki-Yoon Kim indicated no relevant financial relationships.
Franklin Tsai indicated no relevant financial relationships.
Walter Coyle indicated no relevant financial relationships.
Matthew Skinner: Boston Scientific – Consultant.
Ki-Yoon Kim, MD1, Franklin Tsai, MD2, Walter Coyle, MD2, Matthew J. Skinner, MD2. A0444 - Endoscopic Management of Dumping Syndrome in a Roux-en-Y Gastric Bypass (RYGB) Patient With Transoral Outlet Reduction and Remnant Stomach Access With Lumen Apposing Metal Stent, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
