Back

Poster Session A - Sunday Afternoon
Category: Esophagus
A0227 - The Great Mimicker: Esophageal Sarcoidosis Masquerading as Malignancy
Sunday, October 23, 2022
5:00 PM – 7:00 PM ET
Location: Crown Ballroom
Has Audio
- AK
Andree H. Koop, MD
Mayo Clinic
Jacksonville, Florida
Presenting Author(s)
Andree H. Koop, MD1, Atulya Khosla, MBBS1, Bhaumik Brahmbhatt, MD2
1Mayo Clinic, Jacksonville, FL; 2Mayo Clinic Jacksonville, Jacksonville, FL
Introduction: Sarcoidosis is a chronic, multi-system disorder that most commonly affects the lungs. Luminal gastrointestinal involvement including the esophagus is rare, occurring in less than 2% of patients. We describe a case not previously reported of esophageal sarcoidosis presenting as a cratered, esophageal ulcer concerning for malignancy.
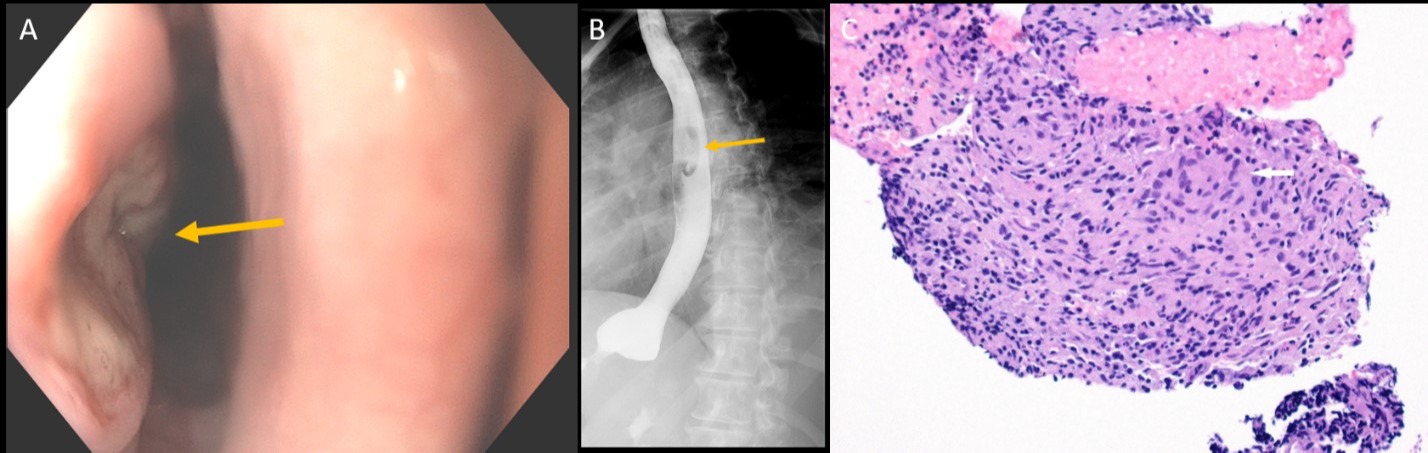
Case Description/Methods: A 43-year-old woman presented to clinic with three months of solid food dysphagia and epigastric pain. Her medical history was notable for laparoscopic Roux-en-Y gastric bypass surgery two years earlier. Esophagogastroduodenoscopy (EGD) demonstrated a large, cratered ulcer with irregular borders in the mid esophagus concerning for malignancy (Figure A). The ulcer was deep with concern for an underlying fistula, and esophageal biopsies were deferred until further imaging was performed. Esophagram showed a 3 cm ovoid filling defect in the anterolateral mid-thoracic esophagus with surrounding edema. Computed tomography scan of the chest demonstrated a subcarinal soft tissue mass adjacent to the right esophageal wall measuring 21x27x47 mm, difficult to distinguish from surrounding posterior mediastinal lymph nodes. There was prominent mediastinal lymphadenopathy. Esophagogastroduodenoscopy with endoscopic ultrasound showed a 17x40 mm non-circumferential, hypoechoic, and heterogeneous mass with invasion of the esophageal wall from the adventitia through the mucosa, which appeared consistent with a large lymph node. Pathology showed multiple non-necrotizing granulomas consistent with sarcoidosis. The patient was referred to Rheumatology and due to prior intolerance to prednisone (severe psychosis), treated with mycophenolate mofetil and close follow-up in clinic.
Discussion: This is a rare presentation of esophageal sarcoidosis presenting as a large, cratered esophageal ulcer concerning for malignancy. Esophageal sarcoidosis most often presents with dysphagia that can occur secondary to mucosal involvement with stricture or mass, infiltration of the myenteric plexus and associated dysmotility, or external compression from lymphadenopathy. Corticosteroids are the primary treatment, and the duration of therapy depends on the clinical response. In patients with atypical endoscopic findings including mucosal lesions, strictures, or ulcers, sarcoidosis should be considered.
Disclosures:
Andree H. Koop, MD1, Atulya Khosla, MBBS1, Bhaumik Brahmbhatt, MD2. A0227 - The Great Mimicker: Esophageal Sarcoidosis Masquerading as Malignancy, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1Mayo Clinic, Jacksonville, FL; 2Mayo Clinic Jacksonville, Jacksonville, FL
Introduction: Sarcoidosis is a chronic, multi-system disorder that most commonly affects the lungs. Luminal gastrointestinal involvement including the esophagus is rare, occurring in less than 2% of patients. We describe a case not previously reported of esophageal sarcoidosis presenting as a cratered, esophageal ulcer concerning for malignancy.
Case Description/Methods: A 43-year-old woman presented to clinic with three months of solid food dysphagia and epigastric pain. Her medical history was notable for laparoscopic Roux-en-Y gastric bypass surgery two years earlier. Esophagogastroduodenoscopy (EGD) demonstrated a large, cratered ulcer with irregular borders in the mid esophagus concerning for malignancy (Figure A). The ulcer was deep with concern for an underlying fistula, and esophageal biopsies were deferred until further imaging was performed. Esophagram showed a 3 cm ovoid filling defect in the anterolateral mid-thoracic esophagus with surrounding edema. Computed tomography scan of the chest demonstrated a subcarinal soft tissue mass adjacent to the right esophageal wall measuring 21x27x47 mm, difficult to distinguish from surrounding posterior mediastinal lymph nodes. There was prominent mediastinal lymphadenopathy. Esophagogastroduodenoscopy with endoscopic ultrasound showed a 17x40 mm non-circumferential, hypoechoic, and heterogeneous mass with invasion of the esophageal wall from the adventitia through the mucosa, which appeared consistent with a large lymph node. Pathology showed multiple non-necrotizing granulomas consistent with sarcoidosis. The patient was referred to Rheumatology and due to prior intolerance to prednisone (severe psychosis), treated with mycophenolate mofetil and close follow-up in clinic.
Discussion: This is a rare presentation of esophageal sarcoidosis presenting as a large, cratered esophageal ulcer concerning for malignancy. Esophageal sarcoidosis most often presents with dysphagia that can occur secondary to mucosal involvement with stricture or mass, infiltration of the myenteric plexus and associated dysmotility, or external compression from lymphadenopathy. Corticosteroids are the primary treatment, and the duration of therapy depends on the clinical response. In patients with atypical endoscopic findings including mucosal lesions, strictures, or ulcers, sarcoidosis should be considered.
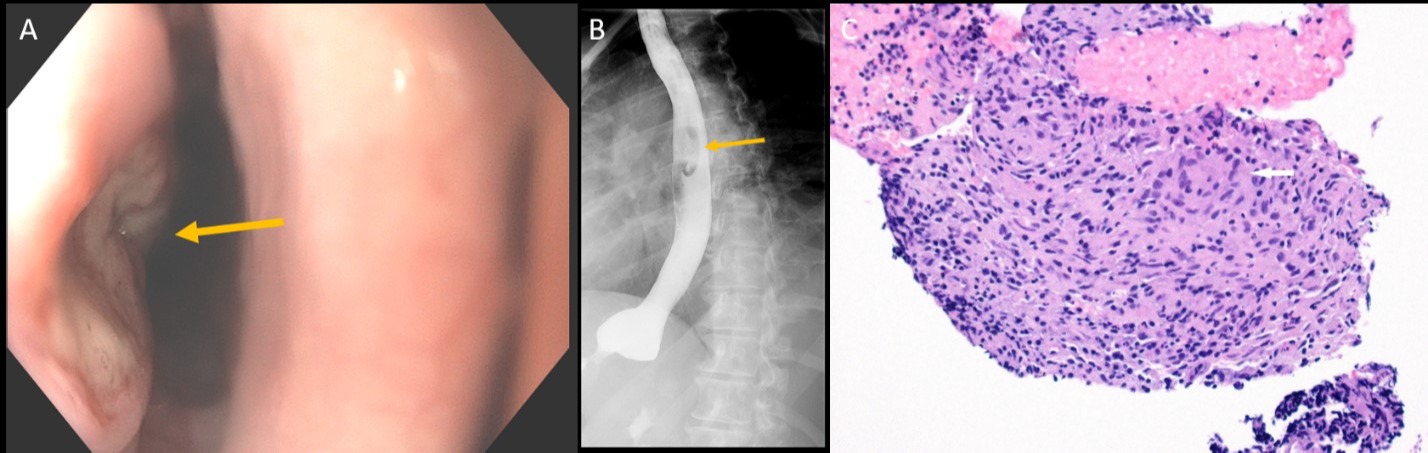
Figure: Figure A: Image from esophagogastroduodenoscopy of a large, cratered ulcer (arrow) in the middle esophagus. Figure B: Fluoroscopic images from esophagram demonstrating an irregular, ovoid shaped filling defect consistent with ulcer (arrow) in the mid esophagus. Figure C: Microscopic image from endoscopic ultrasound-guided fine needle biopsy of the mediastinal lesion demonstrating a non-necrotizing granuloma with a multinucleated giant cell (arrow). Hematoxylin and eosin stain; original magnification x 200.
Disclosures:
Andree Koop indicated no relevant financial relationships.
Atulya Khosla indicated no relevant financial relationships.
Bhaumik Brahmbhatt indicated no relevant financial relationships.
Andree H. Koop, MD1, Atulya Khosla, MBBS1, Bhaumik Brahmbhatt, MD2. A0227 - The Great Mimicker: Esophageal Sarcoidosis Masquerading as Malignancy, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
