Back

Poster Session D - Tuesday Morning
Category: GI Bleeding
D0332 - Gastroduodenal Artery Aneurysm: When Endoscopy Is Not the Answer
Tuesday, October 25, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom
Has Audio
- JK
Jacyln E. Kagihara, MD
George Washington University
Washington, DC
Presenting Author(s)
Jaclyn E. Kagihara, MD, Justin P. Canakis, DO, Francis Carro Cruz, MD, Marie L. Borum, MD, EdD, MPH, Samuel A. Schueler, MD
George Washington University, Washington, DC
Introduction: Gastroduodenal artery aneurysms (GDAAs) are rare with high mortality rate. We present a patient with massive gastrointestinal (GI) bleeding found to have gastroduodenal artery pseudoaneurysm.
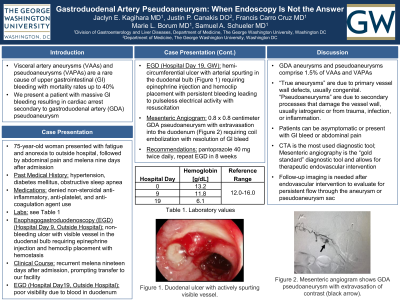
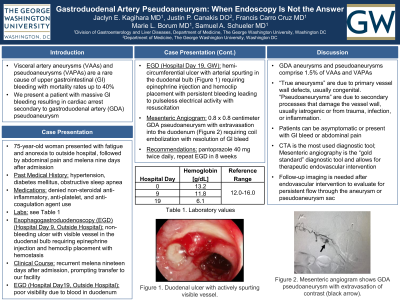
Case Description/Methods: A 75-year-old woman with hypertension, diabetes, sleep apnea, and prior stroke presented with fatigue, nausea, and decreased appetite. Vital signs and physical exam were normal. Hemoglobin (Hgb) was 13.2 grams per deciliter (g/dl). Nine days later, she developed abdominal pain and melena. Vital signs and physical exam were normal, Hgb was 11.8 g/dl, and computed tomography angiography (CTA) was normal. Esophagogastroduodenoscopy (EGD) showed duodenal ulcer with visible vessel, treated with epinephrine injection (epi) and hemoclips. Melena recurred eleven days later. Repeat EGD showed duodenal bleeding with poor visibility, prompting transfer to our hospital. EGD at our facility showed hemi-circumferential deep ulcer and arterial spurting in the distal duodenal bulb, treated with epi and hemoclips resulting in initial hemostasis but then continued bleeding (Figure 1A). She developed pulseless electrical activity arrest but was resuscitated. Mesenteric angiogram showed a 0.8 x 0.8 centimeter distal gastroduodenal artery pseudoaneurysm with extravasation requiring embolization with 2-4 millimeter interlock coils (Figure 1B). There was no further bleeding and she was discharged.
Discussion: GDAAs account for 1.5% of visceral arterial aneurysms, which include true aneurysms and pseudoaneurysms (PAs). True aneurysms arise from vessel wall abnormalities such as degenerative or atherosclerotic processes, fibromuscular dysplasia, or collagen vascular diseases. PAs arise from vascular insults such as trauma, iatrogenic injury, or inflammation. The risk of GDAA PA rupture is as high as 75%. GDAAs may be asymptomatic or present as GI bleeding, abdominal pain, gastric outlet obstruction, or a pulsatile abdominal mass. CTA is the initial imaging of choice given high sensitivity, availability, and promptness. Mesenteric angiography is the diagnostic gold standard and allows for therapeutic intervention with endovascular embolization, which has superior outcomes compared to open surgical ligation. Follow-up imaging is necessary to look for aneurysm reperfusion, seen in 9-15% of cases. GDAA rupture is a difficult yet crucial diagnosis to make given mortality rate up to 21%.

Disclosures:
Jaclyn E. Kagihara, MD, Justin P. Canakis, DO, Francis Carro Cruz, MD, Marie L. Borum, MD, EdD, MPH, Samuel A. Schueler, MD. D0332 - Gastroduodenal Artery Aneurysm: When Endoscopy Is Not the Answer, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
George Washington University, Washington, DC
Introduction: Gastroduodenal artery aneurysms (GDAAs) are rare with high mortality rate. We present a patient with massive gastrointestinal (GI) bleeding found to have gastroduodenal artery pseudoaneurysm.
Case Description/Methods: A 75-year-old woman with hypertension, diabetes, sleep apnea, and prior stroke presented with fatigue, nausea, and decreased appetite. Vital signs and physical exam were normal. Hemoglobin (Hgb) was 13.2 grams per deciliter (g/dl). Nine days later, she developed abdominal pain and melena. Vital signs and physical exam were normal, Hgb was 11.8 g/dl, and computed tomography angiography (CTA) was normal. Esophagogastroduodenoscopy (EGD) showed duodenal ulcer with visible vessel, treated with epinephrine injection (epi) and hemoclips. Melena recurred eleven days later. Repeat EGD showed duodenal bleeding with poor visibility, prompting transfer to our hospital. EGD at our facility showed hemi-circumferential deep ulcer and arterial spurting in the distal duodenal bulb, treated with epi and hemoclips resulting in initial hemostasis but then continued bleeding (Figure 1A). She developed pulseless electrical activity arrest but was resuscitated. Mesenteric angiogram showed a 0.8 x 0.8 centimeter distal gastroduodenal artery pseudoaneurysm with extravasation requiring embolization with 2-4 millimeter interlock coils (Figure 1B). There was no further bleeding and she was discharged.
Discussion: GDAAs account for 1.5% of visceral arterial aneurysms, which include true aneurysms and pseudoaneurysms (PAs). True aneurysms arise from vessel wall abnormalities such as degenerative or atherosclerotic processes, fibromuscular dysplasia, or collagen vascular diseases. PAs arise from vascular insults such as trauma, iatrogenic injury, or inflammation. The risk of GDAA PA rupture is as high as 75%. GDAAs may be asymptomatic or present as GI bleeding, abdominal pain, gastric outlet obstruction, or a pulsatile abdominal mass. CTA is the initial imaging of choice given high sensitivity, availability, and promptness. Mesenteric angiography is the diagnostic gold standard and allows for therapeutic intervention with endovascular embolization, which has superior outcomes compared to open surgical ligation. Follow-up imaging is necessary to look for aneurysm reperfusion, seen in 9-15% of cases. GDAA rupture is a difficult yet crucial diagnosis to make given mortality rate up to 21%.

Figure: Figure 1. A, Duodenal ulcer with actively spurting visible vessel. B, Mesenteric angiogram shows gastroduodenal artery pseudoaneurysm with extravasation of contrast (black arrow).
Disclosures:
Jaclyn Kagihara indicated no relevant financial relationships.
Justin Canakis indicated no relevant financial relationships.
Francis Carro Cruz indicated no relevant financial relationships.
Marie Borum: Takeda – Advisory Committee/Board Member.
Samuel Schueler indicated no relevant financial relationships.
Jaclyn E. Kagihara, MD, Justin P. Canakis, DO, Francis Carro Cruz, MD, Marie L. Borum, MD, EdD, MPH, Samuel A. Schueler, MD. D0332 - Gastroduodenal Artery Aneurysm: When Endoscopy Is Not the Answer, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
