Back


Poster Session C - Monday Afternoon
Category: Small Intestine
C0674 - Chronic Diarrhea Caused by Duodenal Diverticulum
Monday, October 24, 2022
3:00 PM – 5:00 PM ET
Location: Crown Ballroom

Has Audio

Pooja J. Mude, DO
Augusta University Medical Center
Augusta, GA
Presenting Author(s)
Pooja J. Mude, DO1, Shreyans Doshi, MD1, Kristin Harper, PA-C1, Karmen Elsen, PA-C1, John Erikson L. Yap, MD2
1Augusta University Medical Center, Augusta, GA; 2Augusta University Medical College of Georiga, Augusta, GA
Introduction: Diverticula are bulging sacs that can occur in any part of the gastrointestinal tract. While mostly seen in the large intestine, 9–23% of small bowel diverticula are found incidentally via endoscopy. Small intestinal bacterial overgrowth (SIBO) is characterized by an abnormally increased bacterial burden in the small intestine with symptoms including abdominal distension and pain, bloating, and diarrhea. Small intestinal diverticulosis is a known risk factor for SIBO. Small bowel aspirates and culture is considered gold standard for diagnosing SIBO, while aspirates from diverticula is not routine practice for diagnosis. We present a case of SIBO diagnosed by aspirates from a large duodenal diverticulum (DD).
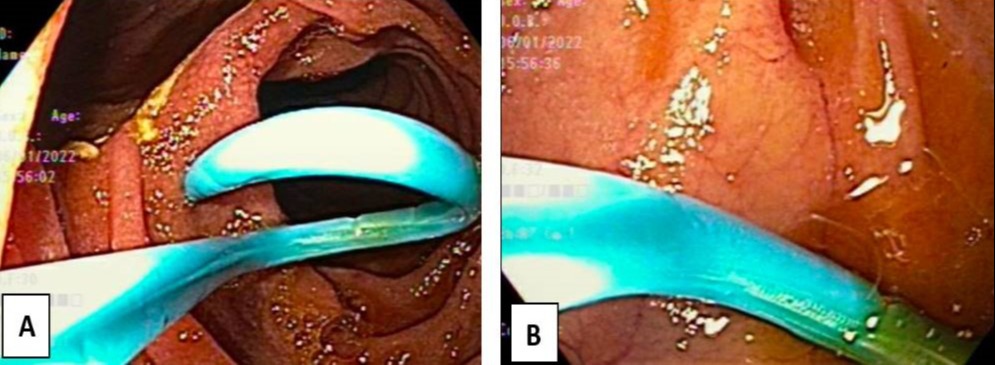
Case Description/Methods: A 62-year-old female with chronic diarrhea, hepatic steatosis without cirrhosis, GERD, and diverticulosis presented to the gastroenterology clinic for continued complaints of diarrhea and bloating. The patient noted 4-5 bowel movements per day. Vital signs, physical exam, and previous workup including stool culture, Clostridium difficile study, colonoscopy with biopsies, fecal calprotectin and elastase, abdominal imaging, and celiac serologies were unremarkable. Patient tried pancrelipase with no noticeable difference in diarrhea. An esophagoduodenoscopy (EGD) performed showed multiple fundic gland polyps in the stomach and a large 40 mm diverticula in the 3rd portion of the duodenum. Duodenal and gastric biopsies obtained ruled out celiac disease, pathogens, and Helicobacter pylori. Aspiration of duodenal diverticular fluid was significant for >100,000 colony forming units per mL (CFU/mL) Escherichia coli, Enterococcus faecium, and Streptococcus mitis. Disaccharidases (lactase, sucrase, maltase, palatinase, glucoamylase) were within normal limits. Patient was initiated on rifaximin 550mg TID for 14 days with improvement of her chronic symptoms.
Discussion: While most DD are asymptomatic, small, and require no treatment, intervention is necessary if the patient develops SIBO, bowel obstruction, diverticulitis, bleeding, or perforation. SIBO can be diagnosed via small bowel aspirates showing >1000 CFU/mL. Large DD can lead to SIBO by creating a protected environment for bacterial species. Treatment of diarrhea due to SIBO and large DDs are treated with antibiotic therapy, like our patient who was prescribed rifaximin and noted improvement of symptoms. It is important to understand that while DD are uncommon, large diverticulum can lead to chronic diarrhea and SIBO.
Disclosures:
Pooja J. Mude, DO1, Shreyans Doshi, MD1, Kristin Harper, PA-C1, Karmen Elsen, PA-C1, John Erikson L. Yap, MD2. C0674 - Chronic Diarrhea Caused by Duodenal Diverticulum, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1Augusta University Medical Center, Augusta, GA; 2Augusta University Medical College of Georiga, Augusta, GA
Introduction: Diverticula are bulging sacs that can occur in any part of the gastrointestinal tract. While mostly seen in the large intestine, 9–23% of small bowel diverticula are found incidentally via endoscopy. Small intestinal bacterial overgrowth (SIBO) is characterized by an abnormally increased bacterial burden in the small intestine with symptoms including abdominal distension and pain, bloating, and diarrhea. Small intestinal diverticulosis is a known risk factor for SIBO. Small bowel aspirates and culture is considered gold standard for diagnosing SIBO, while aspirates from diverticula is not routine practice for diagnosis. We present a case of SIBO diagnosed by aspirates from a large duodenal diverticulum (DD).
Case Description/Methods: A 62-year-old female with chronic diarrhea, hepatic steatosis without cirrhosis, GERD, and diverticulosis presented to the gastroenterology clinic for continued complaints of diarrhea and bloating. The patient noted 4-5 bowel movements per day. Vital signs, physical exam, and previous workup including stool culture, Clostridium difficile study, colonoscopy with biopsies, fecal calprotectin and elastase, abdominal imaging, and celiac serologies were unremarkable. Patient tried pancrelipase with no noticeable difference in diarrhea. An esophagoduodenoscopy (EGD) performed showed multiple fundic gland polyps in the stomach and a large 40 mm diverticula in the 3rd portion of the duodenum. Duodenal and gastric biopsies obtained ruled out celiac disease, pathogens, and Helicobacter pylori. Aspiration of duodenal diverticular fluid was significant for >100,000 colony forming units per mL (CFU/mL) Escherichia coli, Enterococcus faecium, and Streptococcus mitis. Disaccharidases (lactase, sucrase, maltase, palatinase, glucoamylase) were within normal limits. Patient was initiated on rifaximin 550mg TID for 14 days with improvement of her chronic symptoms.
Discussion: While most DD are asymptomatic, small, and require no treatment, intervention is necessary if the patient develops SIBO, bowel obstruction, diverticulitis, bleeding, or perforation. SIBO can be diagnosed via small bowel aspirates showing >1000 CFU/mL. Large DD can lead to SIBO by creating a protected environment for bacterial species. Treatment of diarrhea due to SIBO and large DDs are treated with antibiotic therapy, like our patient who was prescribed rifaximin and noted improvement of symptoms. It is important to understand that while DD are uncommon, large diverticulum can lead to chronic diarrhea and SIBO.
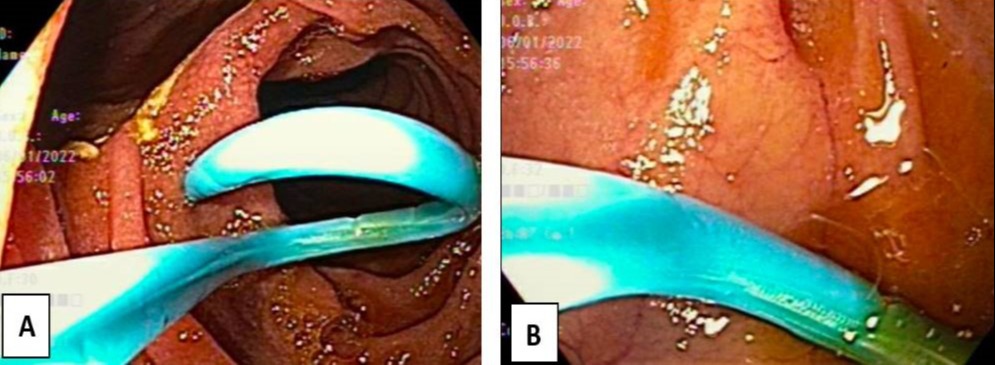
Figure: Image 1: [A] EGD findings with a large duodenal diverticulum in the upper left corner; [B] Process of aspirating duodenal diverticulum fluid.
Disclosures:
Pooja Mude indicated no relevant financial relationships.
Shreyans Doshi indicated no relevant financial relationships.
Kristin Harper indicated no relevant financial relationships.
Karmen Elsen indicated no relevant financial relationships.
John Erikson Yap indicated no relevant financial relationships.
Pooja J. Mude, DO1, Shreyans Doshi, MD1, Kristin Harper, PA-C1, Karmen Elsen, PA-C1, John Erikson L. Yap, MD2. C0674 - Chronic Diarrhea Caused by Duodenal Diverticulum, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
