Back


Poster Session D - Tuesday Morning
Category: IBD
D0391 - Inflammatory Bowel Disease Is a Strong Predictor of Central Line-Associated Blood Stream Infections in Patients Admitted to the ICU
Tuesday, October 25, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom

Has Audio

Mohammad Darweesh, MD
East Tennessee State University
Johnson City, TN
Presenting Author(s)
Mohammad Darweesh, MD1, Rasheed Musa, MD1, Ratib Mahfouz, MD2, Mahmoud Mansour, MD3, Adham E. Obeidat, MBBS4, Usama Abu-Heija, MBBS1, Chakradhar Reddy, MD1
1East Tennessee State University, Johnson City, TN; 2Brown University/Kent Hospital, Providence, RI; 3University of Missouri Columbia, Columbia, MO; 4University of Hawaii, Honolulu, HI
Introduction: Inflammatory bowel disease (IBD) course can be complicated with ICU admission and central line placement for different reasons. One of the common complications of central line placement is central line-associated bloodstream infections (CLABSI).
Methods: A retrospective study was conducted utilizing the Nationwide Inpatient Sample database (NIS) for the years 2016 to 2018. Patients with CLABSI and IBD were identified using ICD 10 diagnosis codes from all listed discharge diagnoses. Patients younger than 18 years of age, and missing information for age, gender, or race were excluded. ICU admission was defined by the presence of vasopressors or mechanical ventilation. Multivariate logistic regression analysis was performed to compare different risk factors in predicting CLABSI.
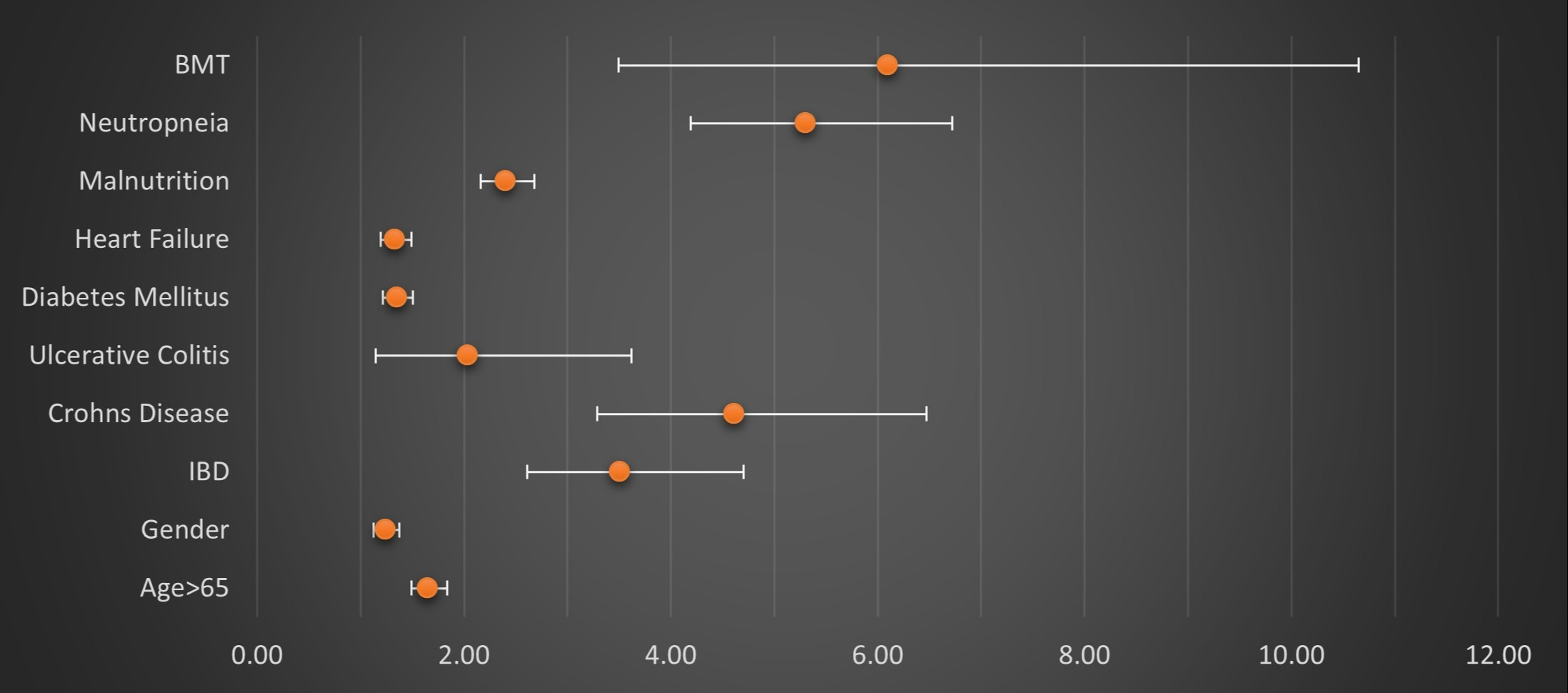
Results: 3,196,820 patients were included in this study, of those; 7924 (0.24%) had CLABSI. This study reports that adults admitted to the ICU had increased odds of developing CLABSI by three and a half times when they had IBD (OR 3.51, P-value 0.00, 95% CI 2.61-4.70), six times when they had bone marrow transplant (OR 6.10, P-value 0.00, 95% CI 3.49-10.65), and five times when they had neutropenia (OR 5.31, P-value 0.00, 95% CI 4.19-6.72), all were statistically significant. Upon subdividing patients with IBD into Crohn’s disease (CD) and ulcerative colitis (UC), we found that patients with CD tend to have high odds of developing CLABSI with OR of 4.61 (P-value 0.00, 95% CI 3.29-6.47) compared to patients with UC who had OR of 2.04 (P-value 0.02, 95% CI 1.15-3.62) and both were statistically significant.
Discussion: This study demonstrates high odds of CLABSI in IBD patients admitted to the ICU compared to patients without such a history. This result can be explained by multiple factors. The fact that patients with IBD are usually treated with immune suppressants can result in a higher incidence of infections including CLABSI. Other etiologies might also include total parenteral nutrition (TPN), as patients with IBD may require TPN as part of their nutritional support while in the ICU. After subdividing patients with IBD into CD and UC, the odds of encountering CLABS tend to be higher in CD, no clear etiology for this finding was found, however, it can be secondary to the transmural involvement of the intestinal wall in CD compared to the submucosal involvement in UC.
Disclosures:
Mohammad Darweesh, MD1, Rasheed Musa, MD1, Ratib Mahfouz, MD2, Mahmoud Mansour, MD3, Adham E. Obeidat, MBBS4, Usama Abu-Heija, MBBS1, Chakradhar Reddy, MD1. D0391 - Inflammatory Bowel Disease Is a Strong Predictor of Central Line-Associated Blood Stream Infections in Patients Admitted to the ICU, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1East Tennessee State University, Johnson City, TN; 2Brown University/Kent Hospital, Providence, RI; 3University of Missouri Columbia, Columbia, MO; 4University of Hawaii, Honolulu, HI
Introduction: Inflammatory bowel disease (IBD) course can be complicated with ICU admission and central line placement for different reasons. One of the common complications of central line placement is central line-associated bloodstream infections (CLABSI).
Methods: A retrospective study was conducted utilizing the Nationwide Inpatient Sample database (NIS) for the years 2016 to 2018. Patients with CLABSI and IBD were identified using ICD 10 diagnosis codes from all listed discharge diagnoses. Patients younger than 18 years of age, and missing information for age, gender, or race were excluded. ICU admission was defined by the presence of vasopressors or mechanical ventilation. Multivariate logistic regression analysis was performed to compare different risk factors in predicting CLABSI.
Results: 3,196,820 patients were included in this study, of those; 7924 (0.24%) had CLABSI. This study reports that adults admitted to the ICU had increased odds of developing CLABSI by three and a half times when they had IBD (OR 3.51, P-value 0.00, 95% CI 2.61-4.70), six times when they had bone marrow transplant (OR 6.10, P-value 0.00, 95% CI 3.49-10.65), and five times when they had neutropenia (OR 5.31, P-value 0.00, 95% CI 4.19-6.72), all were statistically significant. Upon subdividing patients with IBD into Crohn’s disease (CD) and ulcerative colitis (UC), we found that patients with CD tend to have high odds of developing CLABSI with OR of 4.61 (P-value 0.00, 95% CI 3.29-6.47) compared to patients with UC who had OR of 2.04 (P-value 0.02, 95% CI 1.15-3.62) and both were statistically significant.
Discussion: This study demonstrates high odds of CLABSI in IBD patients admitted to the ICU compared to patients without such a history. This result can be explained by multiple factors. The fact that patients with IBD are usually treated with immune suppressants can result in a higher incidence of infections including CLABSI. Other etiologies might also include total parenteral nutrition (TPN), as patients with IBD may require TPN as part of their nutritional support while in the ICU. After subdividing patients with IBD into CD and UC, the odds of encountering CLABS tend to be higher in CD, no clear etiology for this finding was found, however, it can be secondary to the transmural involvement of the intestinal wall in CD compared to the submucosal involvement in UC.
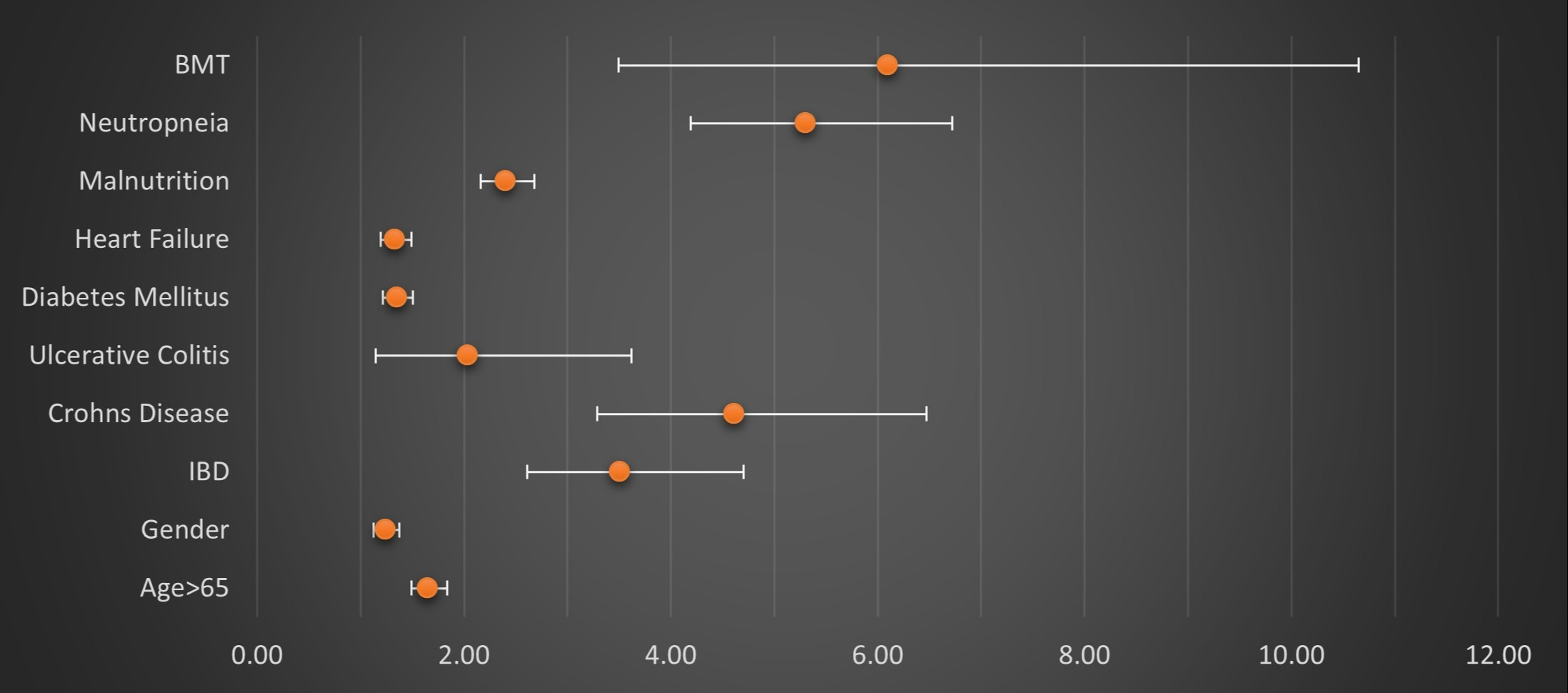
Figure: Figure 1: Multivariate logistic regression analysis representing odds ratios for different predictors of CLABSI in patients admitted to the ICU. BMT: Bone marrow transplant status. IBD: inflammatory bowel disease. CLABSI: catheter-related bloodstream infections.
Disclosures:
Mohammad Darweesh indicated no relevant financial relationships.
Rasheed Musa indicated no relevant financial relationships.
Ratib Mahfouz indicated no relevant financial relationships.
Mahmoud Mansour indicated no relevant financial relationships.
Adham Obeidat indicated no relevant financial relationships.
Usama Abu-Heija indicated no relevant financial relationships.
Chakradhar Reddy indicated no relevant financial relationships.
Mohammad Darweesh, MD1, Rasheed Musa, MD1, Ratib Mahfouz, MD2, Mahmoud Mansour, MD3, Adham E. Obeidat, MBBS4, Usama Abu-Heija, MBBS1, Chakradhar Reddy, MD1. D0391 - Inflammatory Bowel Disease Is a Strong Predictor of Central Line-Associated Blood Stream Infections in Patients Admitted to the ICU, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
