Back

Poster Session A - Sunday Afternoon
Category: Interventional Endoscopy
A0449 - Endoscopic Ultrasound-Guided Drainage of a Remnant Gallbladder
Sunday, October 23, 2022
5:00 PM – 7:00 PM ET
Location: Crown Ballroom
Has Audio
- CF
Chelsea Forbes, MD
Walter Reed National Military Medical Center
Bethesda, MD
Presenting Author(s)
Chelsea Forbes, MD1, Benjamin Fiore, MD2, Michael M. Skaret, MD2, Brian Park, MD2, Joshua McCarron, MD2, Robert Lawson, MD2
1Walter Reed National Military Medical Center, Bethesda, MD; 2Naval Medical Center San Diego, San Diego, CA
Introduction: Endoscopic Ultrasound (EUS) guided drainage of a remnant gallbladder (RGB) with lumen-apposing metal stents (LAMS) can be safely performed for suppurative cholecystitis and choledocholithiasis following subtotal cholecystectomy (STC).
Case Description/Methods: A 68-year-old man presented with recurrent bacteremia secondary to symptomatic RGB after undergoing STC for severe necrotizing gallstone pancreatitis. His preceding course was complicated by infected walled-off pancreatic necrosis, recurrent choledocholithiasis with ascending cholangitis, liver abscess, and bacteremia. His treatments included EUS-guided necrosectomy, multiple endoscopic retrograde cholangiopancreatopgraphies (ERCPs) with unsuccessful attempts at transpapillary gallbladder drainage, and percutaneous cholecystostomy followed by laparoscopic STC. Given his life-threatening complications and poor surgical candidacy EUS-guided drainage of the RGB was pursued.
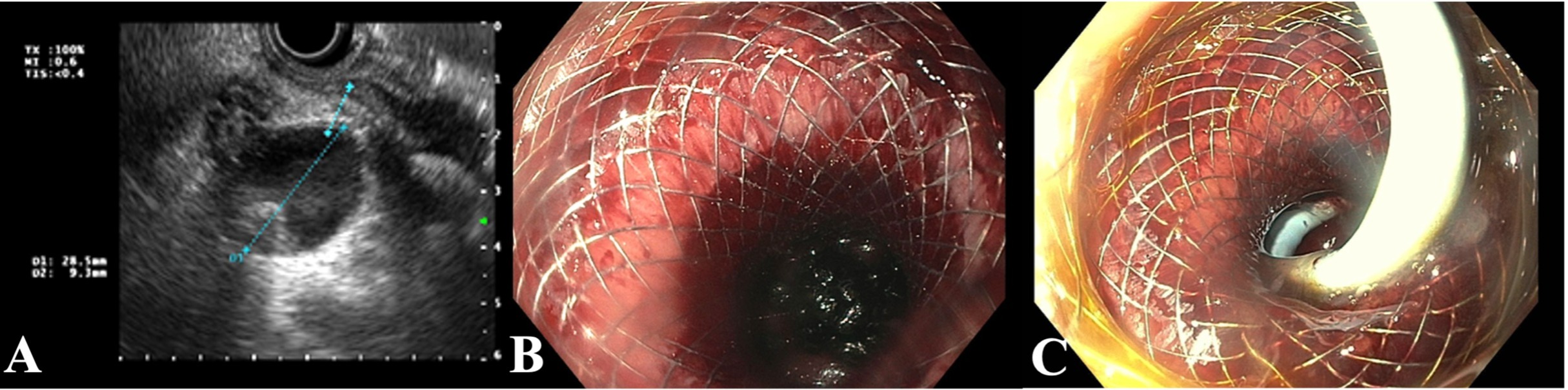
Linear EUS identified the RGB measuring 19.4mm in diameter. Using a 19-gauge FNA needle, the RGB was instilled with 80cc of sterile saline to a diameter of 28.5mm (figure 1a). EUS-guided cholecystogastrostomy was then performed using a 10 x 15 mm electrocautery-enabled access catheter-enhanced LAMS. The LAMS was dilated to 12mm sequentially using a controlled radial expansion balloon. Multiple large, pigmented stones passed with several remaining in the gallbladder (Figure 1b). A 10Fr by 5cm double pigtail stent was passed over a wire into the gallbladder to complete the procedure (Figure 1c).
At one month follow-up ERCP, the LAMS was removed leaving a mature gastrocholecystic fistula. No recurrence of symptoms noted at 12-month follow-up.
Discussion: Laparoscopic cholecystectomy after recovery of gallstone pancreatitis is recommended to reduce risk of recurrent pancreatitis. In some patients, difficult anatomy and inflammation necessitates STC to avoid injury to the extrahepatic bile ducts and surrounding blood vessels. STC is associated with significant morbidity. Completion cholecystectomy for symptomatic complications from RBG is recommended if possible. However, our patient was deemed a poor surgical candidate. Transpapillary drainage of the RBG was also precluded by difficult anatomy with sharp angulation at the confluence of the common hepatic and cystic ducts. This case describes the novel application of EUS-guided drainage of an RBG as a safe and effective alternative to completion cholecystectomy for patients who are poor operative candidates.
Disclosures:
Chelsea Forbes, MD1, Benjamin Fiore, MD2, Michael M. Skaret, MD2, Brian Park, MD2, Joshua McCarron, MD2, Robert Lawson, MD2. A0449 - Endoscopic Ultrasound-Guided Drainage of a Remnant Gallbladder, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1Walter Reed National Military Medical Center, Bethesda, MD; 2Naval Medical Center San Diego, San Diego, CA
Introduction: Endoscopic Ultrasound (EUS) guided drainage of a remnant gallbladder (RGB) with lumen-apposing metal stents (LAMS) can be safely performed for suppurative cholecystitis and choledocholithiasis following subtotal cholecystectomy (STC).
Case Description/Methods: A 68-year-old man presented with recurrent bacteremia secondary to symptomatic RGB after undergoing STC for severe necrotizing gallstone pancreatitis. His preceding course was complicated by infected walled-off pancreatic necrosis, recurrent choledocholithiasis with ascending cholangitis, liver abscess, and bacteremia. His treatments included EUS-guided necrosectomy, multiple endoscopic retrograde cholangiopancreatopgraphies (ERCPs) with unsuccessful attempts at transpapillary gallbladder drainage, and percutaneous cholecystostomy followed by laparoscopic STC. Given his life-threatening complications and poor surgical candidacy EUS-guided drainage of the RGB was pursued.
Linear EUS identified the RGB measuring 19.4mm in diameter. Using a 19-gauge FNA needle, the RGB was instilled with 80cc of sterile saline to a diameter of 28.5mm (figure 1a). EUS-guided cholecystogastrostomy was then performed using a 10 x 15 mm electrocautery-enabled access catheter-enhanced LAMS. The LAMS was dilated to 12mm sequentially using a controlled radial expansion balloon. Multiple large, pigmented stones passed with several remaining in the gallbladder (Figure 1b). A 10Fr by 5cm double pigtail stent was passed over a wire into the gallbladder to complete the procedure (Figure 1c).
At one month follow-up ERCP, the LAMS was removed leaving a mature gastrocholecystic fistula. No recurrence of symptoms noted at 12-month follow-up.
Discussion: Laparoscopic cholecystectomy after recovery of gallstone pancreatitis is recommended to reduce risk of recurrent pancreatitis. In some patients, difficult anatomy and inflammation necessitates STC to avoid injury to the extrahepatic bile ducts and surrounding blood vessels. STC is associated with significant morbidity. Completion cholecystectomy for symptomatic complications from RBG is recommended if possible. However, our patient was deemed a poor surgical candidate. Transpapillary drainage of the RBG was also precluded by difficult anatomy with sharp angulation at the confluence of the common hepatic and cystic ducts. This case describes the novel application of EUS-guided drainage of an RBG as a safe and effective alternative to completion cholecystectomy for patients who are poor operative candidates.
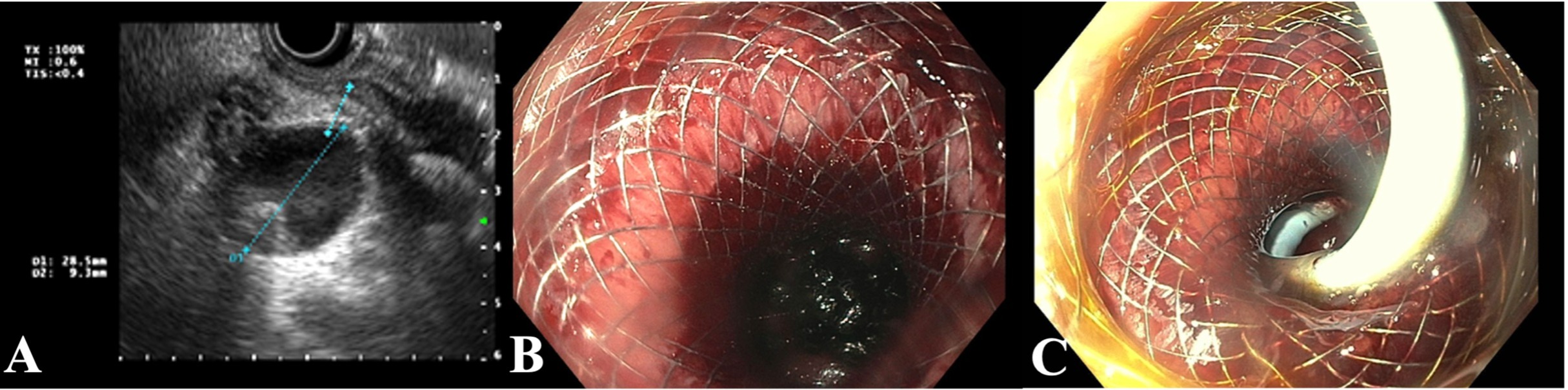
Figure: EUS used to measure dimensions of remnant gallbladder after injecting 80mL of sterile saline (Figure A). Cholecystogastrostomy was performed using a 10 mm X 15 mm LAMS with cautery tip over a wire and dilated using a controlled radial expansion balloon (Figure B). A double pigtail stent was placed through the lumen of the LAMS (Figure C).
Disclosures:
Chelsea Forbes indicated no relevant financial relationships.
Benjamin Fiore indicated no relevant financial relationships.
Michael Skaret indicated no relevant financial relationships.
Brian Park indicated no relevant financial relationships.
Joshua McCarron indicated no relevant financial relationships.
Robert Lawson indicated no relevant financial relationships.
Chelsea Forbes, MD1, Benjamin Fiore, MD2, Michael M. Skaret, MD2, Brian Park, MD2, Joshua McCarron, MD2, Robert Lawson, MD2. A0449 - Endoscopic Ultrasound-Guided Drainage of a Remnant Gallbladder, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
