Back

Poster Session D - Tuesday Morning
Category: Esophagus
D0220 - A Rare Case of Diffuse Esophageal Ulceration in a Patient With a Recent Viral Illness
Tuesday, October 25, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom
Has Audio

Omar Calderon, Jr., MD
University of South Florida
Tampa, FL
Presenting Author(s)
Omar Calderon, MD1, Liza Plafsky, MD1, Rene D. Gomez-Esquivel, MD2
1University of South Florida, Tampa, FL; 2USF Health Morsani College of Medicine, Tampa, FL
Introduction: Pemphigus vulgarism (PV) is an autoimmune bullous disorder involving skin and mucous membranes. PV is rare, especially when it primarily involves the oropharynx and esophagus. Per the literature review, it is an under-diagnosed etiology of odynophagia and can progress to severe ulceration, upper gastrointestinal bleeding, strictures, and increased morbidity and mortality. We present a case of PV manifesting with oropharyngeal and esophageal disease.
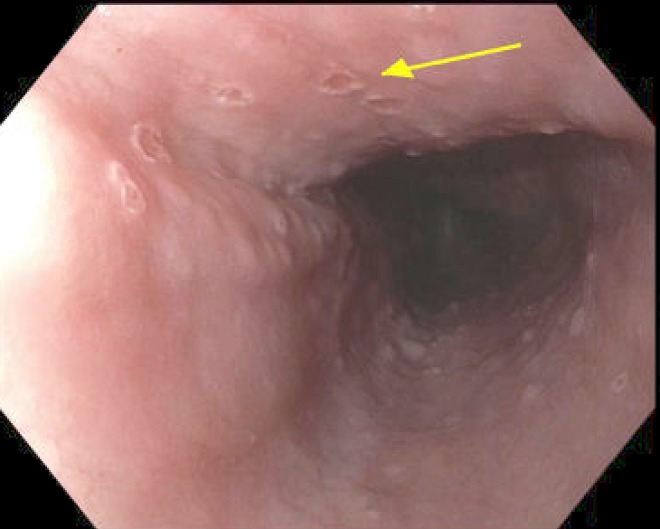
Case Description/Methods: A 47-year-old male with a history of hypertension presented to the emergency department (ED) for painful swallowing for the past three weeks. The patient had previously presented to a dentist for a tooth abscess and was prescribed amoxicillin 1,000 milligrams (mg) or 20-milliliter solution every 12 hours for 8 days. The patient then presented to his primary care doctor for oral ulcers and was prescribed acyclovir 400 mg three times a day for 5 days empirically for herpes simplex virus infection. In the ED, the patient was afebrile and hemodynamically stable. The exam was notable for multiple friable erythematous macules on the buccal mucosa and oropharynx. Labs were significant for mild leukocytosis and acute kidney injury. Microbiology was significant for influenza B. Imaging with CT soft tissue neck without contrast was negative for abnormalities. Upper endoscopy was significant for diffuse ulceration throughout the larynx and esophagus with clean-based circular ulcers, gastritis, and duodenitis. Pathology was significant for acantholysis and H. Pylori but negative for HSV and CMV. Dermatology recommended repeat biopsy with Michel’s solution for examination under direct immunofluorescence. Repeat biopsies were positive for granular immunoglobulin G at interspinous processes and serology was positive for desmoglein 1 and 3. The patient was initiated on prednisone and Rituxan for PV with esophageal involvement.
Discussion: PV with primarily esophageal involvement is exceedingly rare and is associated with increased morbidity and mortality due to delay in diagnosis. It can affect patients that are not immunocompromised, as in this case. Despite multiple evaluations by providers and initial endoscopy, a second endoscopy and consultation with dermatology were required to confirm the diagnosis. This case helps to illustrate the importance of considering PV in the differential for patients with acute odynophagia with ulceration after a viral illness and the use of Michel’s solution for examination under immunofluorescence.
Disclosures:
Omar Calderon, MD1, Liza Plafsky, MD1, Rene D. Gomez-Esquivel, MD2. D0220 - A Rare Case of Diffuse Esophageal Ulceration in a Patient With a Recent Viral Illness, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1University of South Florida, Tampa, FL; 2USF Health Morsani College of Medicine, Tampa, FL
Introduction: Pemphigus vulgarism (PV) is an autoimmune bullous disorder involving skin and mucous membranes. PV is rare, especially when it primarily involves the oropharynx and esophagus. Per the literature review, it is an under-diagnosed etiology of odynophagia and can progress to severe ulceration, upper gastrointestinal bleeding, strictures, and increased morbidity and mortality. We present a case of PV manifesting with oropharyngeal and esophageal disease.
Case Description/Methods: A 47-year-old male with a history of hypertension presented to the emergency department (ED) for painful swallowing for the past three weeks. The patient had previously presented to a dentist for a tooth abscess and was prescribed amoxicillin 1,000 milligrams (mg) or 20-milliliter solution every 12 hours for 8 days. The patient then presented to his primary care doctor for oral ulcers and was prescribed acyclovir 400 mg three times a day for 5 days empirically for herpes simplex virus infection. In the ED, the patient was afebrile and hemodynamically stable. The exam was notable for multiple friable erythematous macules on the buccal mucosa and oropharynx. Labs were significant for mild leukocytosis and acute kidney injury. Microbiology was significant for influenza B. Imaging with CT soft tissue neck without contrast was negative for abnormalities. Upper endoscopy was significant for diffuse ulceration throughout the larynx and esophagus with clean-based circular ulcers, gastritis, and duodenitis. Pathology was significant for acantholysis and H. Pylori but negative for HSV and CMV. Dermatology recommended repeat biopsy with Michel’s solution for examination under direct immunofluorescence. Repeat biopsies were positive for granular immunoglobulin G at interspinous processes and serology was positive for desmoglein 1 and 3. The patient was initiated on prednisone and Rituxan for PV with esophageal involvement.
Discussion: PV with primarily esophageal involvement is exceedingly rare and is associated with increased morbidity and mortality due to delay in diagnosis. It can affect patients that are not immunocompromised, as in this case. Despite multiple evaluations by providers and initial endoscopy, a second endoscopy and consultation with dermatology were required to confirm the diagnosis. This case helps to illustrate the importance of considering PV in the differential for patients with acute odynophagia with ulceration after a viral illness and the use of Michel’s solution for examination under immunofluorescence.
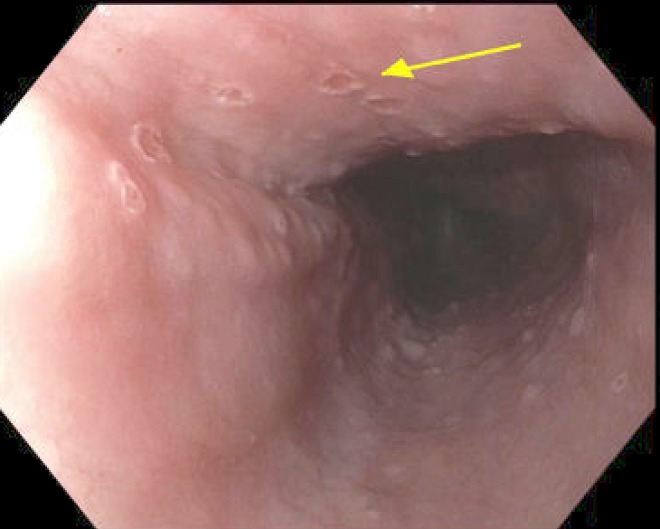
Figure: Well circumscribed clean-based ulcers throughout the esophagus, measuring 2-3 mm with slightly raised borders.
Disclosures:
Omar Calderon indicated no relevant financial relationships.
Liza Plafsky indicated no relevant financial relationships.
Rene Gomez-Esquivel indicated no relevant financial relationships.
Omar Calderon, MD1, Liza Plafsky, MD1, Rene D. Gomez-Esquivel, MD2. D0220 - A Rare Case of Diffuse Esophageal Ulceration in a Patient With a Recent Viral Illness, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
