Back

Poster Session D - Tuesday Morning
Category: Liver
D0507 - Pharmacotherapy for Primary Biliary Cholangitis: An Assessment of Medication Candidacy and Rates of Treatment
Tuesday, October 25, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom
Has Audio
- NM
Nicholas J. MacDonald, MD
Thomas Jefferson University Hospital
Philadelphia, PA
Presenting Author(s)
Nicholas J. MacDonald, MD, Rebecca Loh, MD, Jonathan M. Fenkel, MD, David A. Sass, MD, Dina Halegoua-DeMarzio, MD
Thomas Jefferson University Hospital, Philadelphia, PA
Introduction: Numerous trials have shown that Ursodeoxycholic Acid (UDCA) is effective in improving biochemical indices, delaying progression, and improving survival in patients diagnosed with Primary Biliary Cholangitis (PBC). The alternative therapy, Obeticholic Acid (OCA), is recommended for patients who cannot tolerate UDCA or who have an inadequate response to UDCA monotherapy. Despite the efficacy of these medications, prior investigations suggest that as many as 30% of patients with PBC may have never received treatment. This study aims to characterize usage rates of UDCA and second-line therapies among patients with PBC at a large urban health system with an academic liver transplant program.
Methods: This was an observational, cross-sectional study. Patients were identified according to the ICD-10 code for PBC (ICD-10-CM: K74.3). All patients with a diagnosis of PBC who had any records within the health system were included. Review of medical records was performed to confirm the diagnosis of PBC (defined by AASLD practice guidelines) and determine which medications had been prescribed for treatment of PBC, as well as candidacy for second-line therapies.
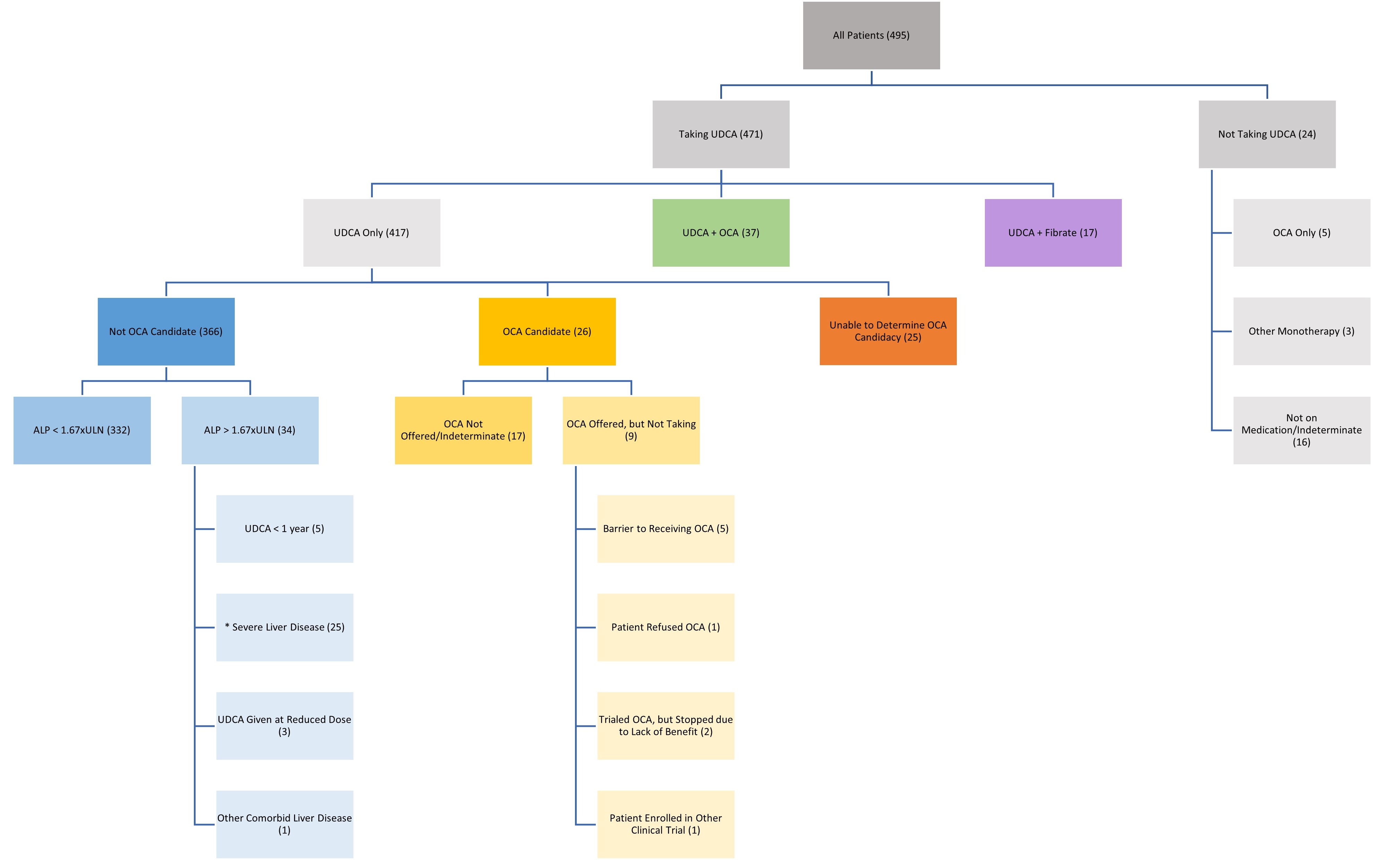
Results: 495 patients met inclusion criteria for this study. Of these, 91% self-identified as female, 7% as male, and 2% did not report. 78% self-identified as white/Caucasian, 7% as black/African American, 3% as Asian, 2% as Hispanic, and 9% did not report. Results for medication candidacy and usage are shown in the attached figure. Notably, 95% of all patients were taking UDCA for treatment of their PBC. 67% of patients had PBC that was well-controlled on UDCA monotherapy. 8% of patients were taking OCA (either as combination or monotherapy). 3% of patients had a persistently elevated alkaline phosphatase despite appropriate treatment with UDCA and would benefit from the addition of OCA but had not been offered the medication. Only 3% of patients were not on any medication for management of PBC.
Discussion: Despite prior investigations suggesting that a large proportion of PBC patients may be unmedicated for the disease, the data presented here suggest that PBC patients are generally being managed according to guidelines in our health system. The majority of patients have disease that is well-controlled with UDCA monotherapy. However, OCA remains an important adjunctive/alternative therapy in certain cases, and physicians should be aware of indications for its use.
Disclosures:
Nicholas J. MacDonald, MD, Rebecca Loh, MD, Jonathan M. Fenkel, MD, David A. Sass, MD, Dina Halegoua-DeMarzio, MD. D0507 - Pharmacotherapy for Primary Biliary Cholangitis: An Assessment of Medication Candidacy and Rates of Treatment, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
Thomas Jefferson University Hospital, Philadelphia, PA
Introduction: Numerous trials have shown that Ursodeoxycholic Acid (UDCA) is effective in improving biochemical indices, delaying progression, and improving survival in patients diagnosed with Primary Biliary Cholangitis (PBC). The alternative therapy, Obeticholic Acid (OCA), is recommended for patients who cannot tolerate UDCA or who have an inadequate response to UDCA monotherapy. Despite the efficacy of these medications, prior investigations suggest that as many as 30% of patients with PBC may have never received treatment. This study aims to characterize usage rates of UDCA and second-line therapies among patients with PBC at a large urban health system with an academic liver transplant program.
Methods: This was an observational, cross-sectional study. Patients were identified according to the ICD-10 code for PBC (ICD-10-CM: K74.3). All patients with a diagnosis of PBC who had any records within the health system were included. Review of medical records was performed to confirm the diagnosis of PBC (defined by AASLD practice guidelines) and determine which medications had been prescribed for treatment of PBC, as well as candidacy for second-line therapies.
Results: 495 patients met inclusion criteria for this study. Of these, 91% self-identified as female, 7% as male, and 2% did not report. 78% self-identified as white/Caucasian, 7% as black/African American, 3% as Asian, 2% as Hispanic, and 9% did not report. Results for medication candidacy and usage are shown in the attached figure. Notably, 95% of all patients were taking UDCA for treatment of their PBC. 67% of patients had PBC that was well-controlled on UDCA monotherapy. 8% of patients were taking OCA (either as combination or monotherapy). 3% of patients had a persistently elevated alkaline phosphatase despite appropriate treatment with UDCA and would benefit from the addition of OCA but had not been offered the medication. Only 3% of patients were not on any medication for management of PBC.
Discussion: Despite prior investigations suggesting that a large proportion of PBC patients may be unmedicated for the disease, the data presented here suggest that PBC patients are generally being managed according to guidelines in our health system. The majority of patients have disease that is well-controlled with UDCA monotherapy. However, OCA remains an important adjunctive/alternative therapy in certain cases, and physicians should be aware of indications for its use.
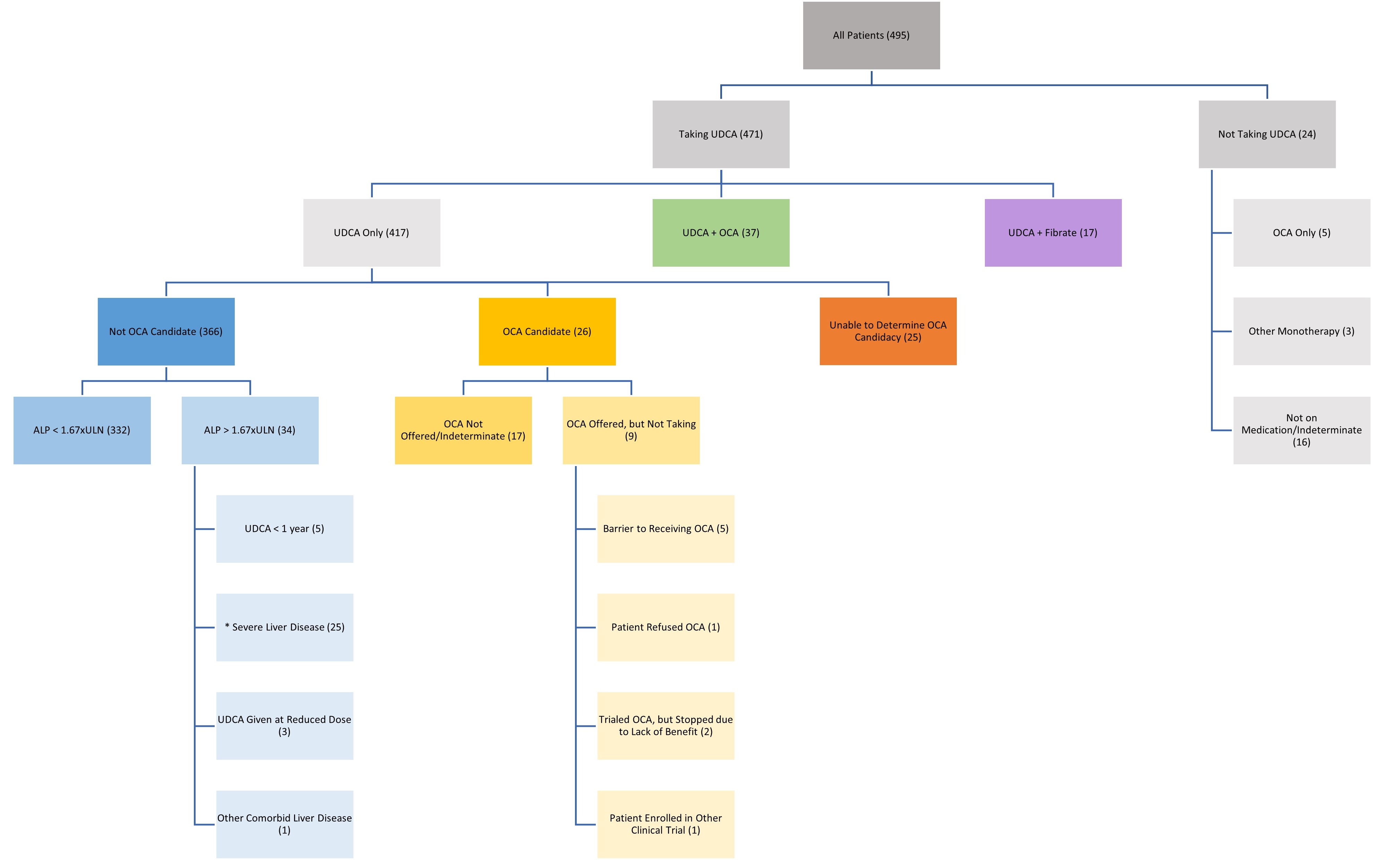
Figure: Medication candidacy and usage among patients diagnosed with PBC.
UDCA – Ursodeoxycholic Acid; OCA – Obeticholic Acid; ALP – Alkaline Phosphatase; ULN – Upper Limit of Normal.
Shown are all patients with a diagnosis of PBC who have records within the health system. Patients were stratified on the basis of medication usage and candidacy for OCA. The number of patients in each category is displayed in parentheses. OCA candidacy is considered to be one or more of the following: failure of ALP to decrease to within 1.67 times the upper limit of normal after one year of therapy with UDCA at appropriate weight-based dosing; inability to tolerate UDCA at appropriate weight-based dosing.
* Severe liver disease is defined as one or more of the following: Child-Pugh B/C categorization; presence of portal hypertension; history of liver decompensation. Severe liver disease is a contraindication to the use of OCA.
UDCA – Ursodeoxycholic Acid; OCA – Obeticholic Acid; ALP – Alkaline Phosphatase; ULN – Upper Limit of Normal.
Shown are all patients with a diagnosis of PBC who have records within the health system. Patients were stratified on the basis of medication usage and candidacy for OCA. The number of patients in each category is displayed in parentheses. OCA candidacy is considered to be one or more of the following: failure of ALP to decrease to within 1.67 times the upper limit of normal after one year of therapy with UDCA at appropriate weight-based dosing; inability to tolerate UDCA at appropriate weight-based dosing.
* Severe liver disease is defined as one or more of the following: Child-Pugh B/C categorization; presence of portal hypertension; history of liver decompensation. Severe liver disease is a contraindication to the use of OCA.
Disclosures:
Nicholas MacDonald indicated no relevant financial relationships.
Rebecca Loh indicated no relevant financial relationships.
Jonathan Fenkel indicated no relevant financial relationships.
David Sass indicated no relevant financial relationships.
Dina Halegoua-DeMarzio indicated no relevant financial relationships.
Nicholas J. MacDonald, MD, Rebecca Loh, MD, Jonathan M. Fenkel, MD, David A. Sass, MD, Dina Halegoua-DeMarzio, MD. D0507 - Pharmacotherapy for Primary Biliary Cholangitis: An Assessment of Medication Candidacy and Rates of Treatment, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
