Back

Poster Session D - Tuesday Morning
Category: Liver
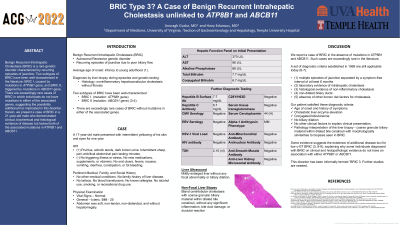
D0526 - BRIC Type 3? A Case of Benign Recurrent Intrahepatic Cholestasis Unlinked to ATP8B1 and ABCB11
Tuesday, October 25, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom
Has Audio
Anuragh Gudur, MD
University of Virginia
Charlottesville, VA
Presenting Author(s)
Anuragh Gudur, MD1, Hany Eskarous, MD2
1University of Virginia, Charlottesville, VA; 2Temple University, Philadelphia, PA
Introduction: Benign Recurrent Intrahepatic Cholestasis (BRIC) is a genetic disorder with two common subtypes: BRIC I (mutated ATP8B1 gene), and BRIC II (mutated ABCB11 gene). Diagnosis requires high degree of suspicion and is confirmed by genetic testing. There are rare cases where patients lack both of the typical mutations. We present a patient with clinical, lab and histological evidence of BRIC without the usual mutations.
Case Description/Methods: A 17-year-old male with no medical history presented with yellow eyes, pruritus, and acholic stools for six weeks, without triggering illness or stress. He denied fatigue, fevers, rash, dizziness, nausea, vomiting, diarrhea, constipation, arthralgias, melena, hematochezia, or hematemesis. He had no tattoos, blood transfusions, or allergies. He denied medications, alcohol, smoking, and drug use.
On exam, he was icteric, with normal abdominal exam, and Alkaline Phosphatase 370 U/L, ALT 96 U/L, AST 66 U/L, and conjugated bilirubin of 6.7 mg/dL. Serological tests were normal, including antibodies for hepatitis A/B/C, CMV, EBV, HIV; alpha-1 antitrypsin; ceruloplasmin; iron, transferrin, C28Y/H63D mutations; TSH; antinuclear, anti-smooth muscle, anti-liver kidney microsomal, anti-mitochondrial antibodies; serum tissue transglutaminase; urine chlamydia and gonorrhea. Liver ultrasound had no biliary dilation.
Genetic testing revealed negative ATP8B1 and ABCB11. Nonfocal liver biopsy showed bland cholestasis with coarse granular material in dilated bile canaliculi, compatible with a disorder of intrahepatic cholestasis, with morphologically similarities to biopsies seen in BRIC. He received ursodiol and symptoms improved. He stopped ursodiol after discharge and presented six months later with similar lab abnormalities. Repeat serological workup was normal. He received ursodiol and symptoms resolved again.
Discussion: Diagnostic criteria for BRIC include episodes of jaundice separated by a symptom-free interval of at least six months, lab and histological evidence of non-inflammatory cholestasis, non-dilated biliary ducts, and no other explanatory causes.
Our patient satisfied these diagnostic criteria. Some evidence indicates the presence of additional disease loci for low γ-GT BRIC, explaining why some patients diagnosed with BRIC on clinical and histopathologic evidence lack usual mutations in ATP8B1 or ABCB11. This disorder is informally termed “BRIC 3”; it is unclear which genes are implicated in this form and further research is needed.

Disclosures:
Anuragh Gudur, MD1, Hany Eskarous, MD2. D0526 - BRIC Type 3? A Case of Benign Recurrent Intrahepatic Cholestasis Unlinked to ATP8B1 and ABCB11, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1University of Virginia, Charlottesville, VA; 2Temple University, Philadelphia, PA
Introduction: Benign Recurrent Intrahepatic Cholestasis (BRIC) is a genetic disorder with two common subtypes: BRIC I (mutated ATP8B1 gene), and BRIC II (mutated ABCB11 gene). Diagnosis requires high degree of suspicion and is confirmed by genetic testing. There are rare cases where patients lack both of the typical mutations. We present a patient with clinical, lab and histological evidence of BRIC without the usual mutations.
Case Description/Methods: A 17-year-old male with no medical history presented with yellow eyes, pruritus, and acholic stools for six weeks, without triggering illness or stress. He denied fatigue, fevers, rash, dizziness, nausea, vomiting, diarrhea, constipation, arthralgias, melena, hematochezia, or hematemesis. He had no tattoos, blood transfusions, or allergies. He denied medications, alcohol, smoking, and drug use.
On exam, he was icteric, with normal abdominal exam, and Alkaline Phosphatase 370 U/L, ALT 96 U/L, AST 66 U/L, and conjugated bilirubin of 6.7 mg/dL. Serological tests were normal, including antibodies for hepatitis A/B/C, CMV, EBV, HIV; alpha-1 antitrypsin; ceruloplasmin; iron, transferrin, C28Y/H63D mutations; TSH; antinuclear, anti-smooth muscle, anti-liver kidney microsomal, anti-mitochondrial antibodies; serum tissue transglutaminase; urine chlamydia and gonorrhea. Liver ultrasound had no biliary dilation.
Genetic testing revealed negative ATP8B1 and ABCB11. Nonfocal liver biopsy showed bland cholestasis with coarse granular material in dilated bile canaliculi, compatible with a disorder of intrahepatic cholestasis, with morphologically similarities to biopsies seen in BRIC. He received ursodiol and symptoms improved. He stopped ursodiol after discharge and presented six months later with similar lab abnormalities. Repeat serological workup was normal. He received ursodiol and symptoms resolved again.
Discussion: Diagnostic criteria for BRIC include episodes of jaundice separated by a symptom-free interval of at least six months, lab and histological evidence of non-inflammatory cholestasis, non-dilated biliary ducts, and no other explanatory causes.
Our patient satisfied these diagnostic criteria. Some evidence indicates the presence of additional disease loci for low γ-GT BRIC, explaining why some patients diagnosed with BRIC on clinical and histopathologic evidence lack usual mutations in ATP8B1 or ABCB11. This disorder is informally termed “BRIC 3”; it is unclear which genes are implicated in this form and further research is needed.

Figure: Figure 1. Histopathologic appearance of the liver biopsy. Bland centrilobular cholestasis with coarse granular biliary material within dilated bile canaliculi, without any significant inflammation, bile duct damage, or ductular reaction.
Disclosures:
Anuragh Gudur indicated no relevant financial relationships.
Hany Eskarous indicated no relevant financial relationships.
Anuragh Gudur, MD1, Hany Eskarous, MD2. D0526 - BRIC Type 3? A Case of Benign Recurrent Intrahepatic Cholestasis Unlinked to ATP8B1 and ABCB11, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
