Back

Poster Session A - Sunday Afternoon
Category: Esophagus
A0266 - Not a Regular Gastric Inlet Patch: A Unique Patient With an Ulcerated Heterotopic Gastric Mucosa of the Entire Middle Esophagus
Sunday, October 23, 2022
5:00 PM – 7:00 PM ET
Location: Crown Ballroom
Has Audio
.jpg)
Muhammad F. Ahmed, MD
SUNY Downstate Medical Center
Brooklyn, NY
Presenting Author(s)
Muhammad F. Ahmed, MD1, Yasir Ali, MD2, Andrew Quinn, MD1, Yaniuska Lescaille, MD3, Qi Yu, MD4
1SUNY Downstate Medical Center, Brooklyn, NY; 2Brookdale Hospital Medical Center, Brooklyn, NY; 3Kings County Medical Center, Brooklyn, NY; 4NYC Health + Hospitals/King's County, SUNY Downstate, Brookyn, NY
Introduction: Heterotopic Gastric Mucosa (HGM), the presence of columnar epithelium of the stomach, can be detected in any part of the gastrointestinal (GI) tract. Inlet patch is a relatively common endoscopic finding where HGM is seen in the cervical esophagus. Mid esophageal HGM is an exceedingly rare entity. Finding of HGM in distal esophagus can be challenging since it needs to be differentiated from Barrett’s esophagus (BE), a lesion with high malignant potential. We report a unique patient with a large (10 cm) patch of mid esophageal HGM who presented with upper GI bleeding.
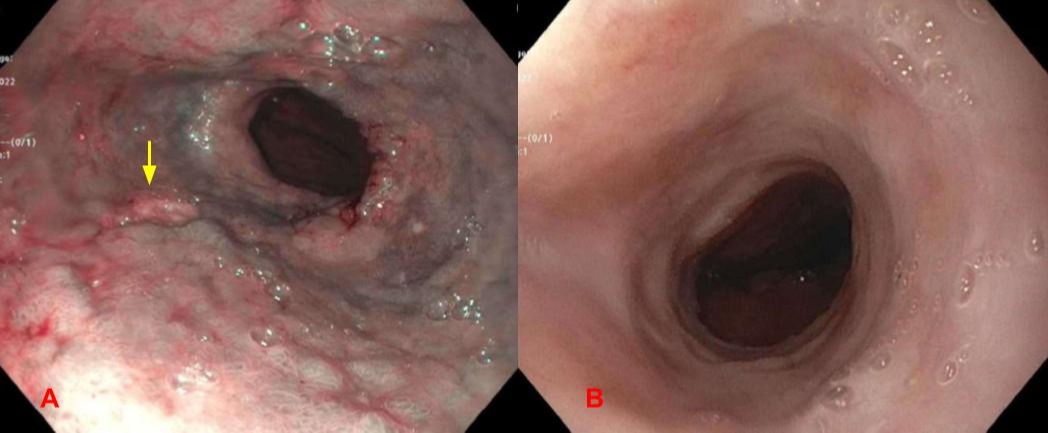
Case Description/Methods: A 82 year old female with history of hypertension and breast cancer presented with shortness of breath and syncope. Patient reported that since 3 weeks she was noticing intermittent liquid black stools. Patient denied taking any non-steroidal anti-inflammatory drugs. Patient also denied any surgical intervention in the abdominal or thoracic cavity. Vitals were unremarkable. Physical exam demonstrated black-tarry liquid stools on rectal exam consistent with melena. Blood work was significant for hemoglobin of 5.9 g/dL with a baseline of 12 g/dL , BUN/Creatinine 68 mg/dL/1.66 mg/dL and with a baseline of 18 mg/dL/1.30 mg/dL. Subsequently patient had an esophagogastroduodenoscopy (EGD) which revealed diffuse salmon-colored mucosa present at 19 to 29 cm from incisors that was erythematous, nodular, friable, and with ulcerations [Fig 1A]. Mucosa was biopsied in a targeted manner in 4 quadrants at intervals of 2 cm. These biopsies demonstrated gastric mucosa with moderate chronic inflammation without any squamous epithelium present. These biopsies were also negative for H. pylori, intestinal metaplasia and dysplasia. Patient was started on Proton pump inhibitor and is planned for a repeat EGD in 3 months to assess for mucosal healing.
Discussion: Mid esophageal heterotopic gastric mucosa is an extremely rare entity which if ulcerated, can lead to life threatening bleeding. Majority of the patients are asymptomatic and diagnosed incidentally when it is complicated with esophageal webs, rings, strictures, fistula, ulcers as in our case, and malignancy. Biopsy plays a key role in differentiating HGM from BE by finding columnar epithelium without intestinal metaplasia or Goblet cells. Treatment is mainly focused on complications seen during endoscopic examination and histopathology. Unlike BE, there are no clear guidelines for the surveillance of HGM since malignant transformation is exceedingly rare.
Disclosures:
Muhammad F. Ahmed, MD1, Yasir Ali, MD2, Andrew Quinn, MD1, Yaniuska Lescaille, MD3, Qi Yu, MD4. A0266 - Not a Regular Gastric Inlet Patch: A Unique Patient With an Ulcerated Heterotopic Gastric Mucosa of the Entire Middle Esophagus, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1SUNY Downstate Medical Center, Brooklyn, NY; 2Brookdale Hospital Medical Center, Brooklyn, NY; 3Kings County Medical Center, Brooklyn, NY; 4NYC Health + Hospitals/King's County, SUNY Downstate, Brookyn, NY
Introduction: Heterotopic Gastric Mucosa (HGM), the presence of columnar epithelium of the stomach, can be detected in any part of the gastrointestinal (GI) tract. Inlet patch is a relatively common endoscopic finding where HGM is seen in the cervical esophagus. Mid esophageal HGM is an exceedingly rare entity. Finding of HGM in distal esophagus can be challenging since it needs to be differentiated from Barrett’s esophagus (BE), a lesion with high malignant potential. We report a unique patient with a large (10 cm) patch of mid esophageal HGM who presented with upper GI bleeding.
Case Description/Methods: A 82 year old female with history of hypertension and breast cancer presented with shortness of breath and syncope. Patient reported that since 3 weeks she was noticing intermittent liquid black stools. Patient denied taking any non-steroidal anti-inflammatory drugs. Patient also denied any surgical intervention in the abdominal or thoracic cavity. Vitals were unremarkable. Physical exam demonstrated black-tarry liquid stools on rectal exam consistent with melena. Blood work was significant for hemoglobin of 5.9 g/dL with a baseline of 12 g/dL , BUN/Creatinine 68 mg/dL/1.66 mg/dL and with a baseline of 18 mg/dL/1.30 mg/dL. Subsequently patient had an esophagogastroduodenoscopy (EGD) which revealed diffuse salmon-colored mucosa present at 19 to 29 cm from incisors that was erythematous, nodular, friable, and with ulcerations [Fig 1A]. Mucosa was biopsied in a targeted manner in 4 quadrants at intervals of 2 cm. These biopsies demonstrated gastric mucosa with moderate chronic inflammation without any squamous epithelium present. These biopsies were also negative for H. pylori, intestinal metaplasia and dysplasia. Patient was started on Proton pump inhibitor and is planned for a repeat EGD in 3 months to assess for mucosal healing.
Discussion: Mid esophageal heterotopic gastric mucosa is an extremely rare entity which if ulcerated, can lead to life threatening bleeding. Majority of the patients are asymptomatic and diagnosed incidentally when it is complicated with esophageal webs, rings, strictures, fistula, ulcers as in our case, and malignancy. Biopsy plays a key role in differentiating HGM from BE by finding columnar epithelium without intestinal metaplasia or Goblet cells. Treatment is mainly focused on complications seen during endoscopic examination and histopathology. Unlike BE, there are no clear guidelines for the surveillance of HGM since malignant transformation is exceedingly rare.
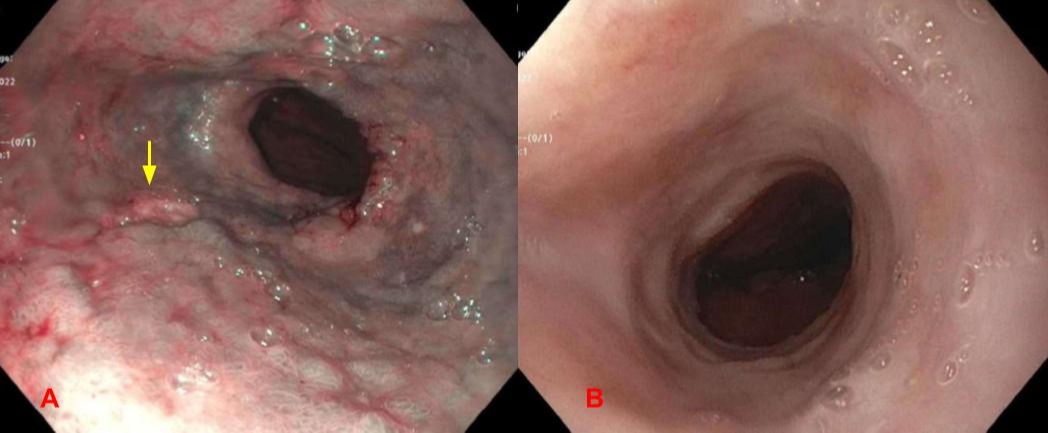
Figure: Fig 1. A) 10cm salmon-colored mucosa in mid esophagus consistent with gastric mucosa without any squamous cells or intestinal metaplasia.The mucosa was erythematous, nodular, and friable with ulcerations (arrow) B) Normal appearing lower esophagus.
Disclosures:
Muhammad Ahmed indicated no relevant financial relationships.
Yasir Ali indicated no relevant financial relationships.
Andrew Quinn indicated no relevant financial relationships.
Yaniuska Lescaille indicated no relevant financial relationships.
Qi Yu indicated no relevant financial relationships.
Muhammad F. Ahmed, MD1, Yasir Ali, MD2, Andrew Quinn, MD1, Yaniuska Lescaille, MD3, Qi Yu, MD4. A0266 - Not a Regular Gastric Inlet Patch: A Unique Patient With an Ulcerated Heterotopic Gastric Mucosa of the Entire Middle Esophagus, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
