Back

Poster Session C - Monday Afternoon
Category: IBD
C0434 - Mesalamine-Induced Interstitial Lung Disease in a Crohn’s Patient With COVID-19
Monday, October 24, 2022
3:00 PM – 5:00 PM ET
Location: Crown Ballroom
Has Audio

Vinay Jahagirdar, MBBS
University of Missouri Kansas City School of Medicine
Kansas City, MO
Presenting Author(s)
Vinay Jahagirdar, MBBS1, Amulya Balagani, MBBS2, Louis Saade, MD3
1University of Missouri Kansas City School of Medicine, Kansas City, MO; 2MedStar Health, Baltimore, MD; 3University of Pittsburgh Medical Center, Pittsburgh, PA
Introduction: Extraintestinal manifestations of Crohn’s disease (CD) generally correlate to the disease activity and may be seen in 1 of 4 patients with CD. Though the prevalence of bronchopulmonary manifestations in CD is 0.4%, subclinical pulmonary changes may be seen in up to half of adults with CD, with involvement of the tracheobronchial tree, lung parenchyma or the pleura.
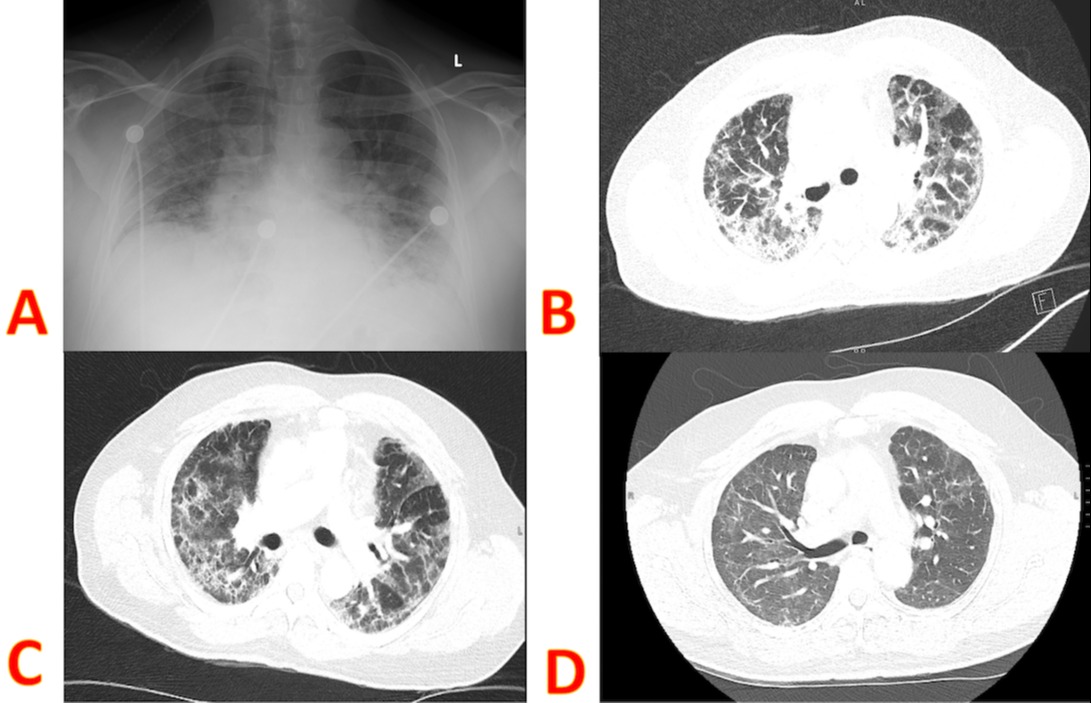
Case Description/Methods: A 61-year-old man, with a history of CD diagnosed 2 years ago, currently in remission with mesalamine, was admitted to the ICU with acute hypoxic respiratory failure due to COVID-19. Inflammatory markers were elevated and he needed high-flow nasal cannula. He was started on a 5-day course of dexamethasone. By HOD-9 O2 requirement and inflammatory markers had trended down. However, around HOD-10 his O2 requirement increased to 6-10 L at rest. CT-chest showed peripherally distributed ground-glass opacities and superimposed early diffuse fibrotic lung changes. Superadded bacterial infection was ruled out. Mesalamine was discontinued and the patient was started on a course of iv methylprednisolone, after which oxygen requirements dramatically declined.
He was discharged on HOD 24 with 2L O2 at rest and 4L on ambulation and a prednisone taper. Chest x-ray in 8 weeks showed improving infiltrates. On follow-up 5 months later, he was not on O2 anymore and was doing well.
Discussion: Latent interstitial pulmonary involvement is seen in around 20%-55% of patients with IBD, with the most common manifestation being drug-induced lung disease, due to sulfasalazine, mesalamine, methotrexate, or anti-TNF agents. Pulmonary function tests can help in early identification of lung injury since respiratory involvement is latent many times. Onset of drug reaction can occur from 5 days to 44 months after initiation of mesalamine therapy and has been reported in the form of eosinophilic pneumonia, organizing pneumonia, nonspecific interstitial pneumonia and hypersensitivity pneumonitis. The absence of other extra-intestinal manifestations, and the remission of CD itself, can be helpful in excluding other pulmonary manifestations of CD from drug-induced lung disease. Discontinuation of the causative drug, along with a course of steroids, can help in reversing the symptoms. Though the differential of mesalamine-induced lung injury, cannot be confirmed nor excluded here, this patient probably had underlying lung pathology from his CD or its treatment, making his recovery from COVID-19 more complicated.
Disclosures:
Vinay Jahagirdar, MBBS1, Amulya Balagani, MBBS2, Louis Saade, MD3. C0434 - Mesalamine-Induced Interstitial Lung Disease in a Crohn’s Patient With COVID-19, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1University of Missouri Kansas City School of Medicine, Kansas City, MO; 2MedStar Health, Baltimore, MD; 3University of Pittsburgh Medical Center, Pittsburgh, PA
Introduction: Extraintestinal manifestations of Crohn’s disease (CD) generally correlate to the disease activity and may be seen in 1 of 4 patients with CD. Though the prevalence of bronchopulmonary manifestations in CD is 0.4%, subclinical pulmonary changes may be seen in up to half of adults with CD, with involvement of the tracheobronchial tree, lung parenchyma or the pleura.
Case Description/Methods: A 61-year-old man, with a history of CD diagnosed 2 years ago, currently in remission with mesalamine, was admitted to the ICU with acute hypoxic respiratory failure due to COVID-19. Inflammatory markers were elevated and he needed high-flow nasal cannula. He was started on a 5-day course of dexamethasone. By HOD-9 O2 requirement and inflammatory markers had trended down. However, around HOD-10 his O2 requirement increased to 6-10 L at rest. CT-chest showed peripherally distributed ground-glass opacities and superimposed early diffuse fibrotic lung changes. Superadded bacterial infection was ruled out. Mesalamine was discontinued and the patient was started on a course of iv methylprednisolone, after which oxygen requirements dramatically declined.
He was discharged on HOD 24 with 2L O2 at rest and 4L on ambulation and a prednisone taper. Chest x-ray in 8 weeks showed improving infiltrates. On follow-up 5 months later, he was not on O2 anymore and was doing well.
Discussion: Latent interstitial pulmonary involvement is seen in around 20%-55% of patients with IBD, with the most common manifestation being drug-induced lung disease, due to sulfasalazine, mesalamine, methotrexate, or anti-TNF agents. Pulmonary function tests can help in early identification of lung injury since respiratory involvement is latent many times. Onset of drug reaction can occur from 5 days to 44 months after initiation of mesalamine therapy and has been reported in the form of eosinophilic pneumonia, organizing pneumonia, nonspecific interstitial pneumonia and hypersensitivity pneumonitis. The absence of other extra-intestinal manifestations, and the remission of CD itself, can be helpful in excluding other pulmonary manifestations of CD from drug-induced lung disease. Discontinuation of the causative drug, along with a course of steroids, can help in reversing the symptoms. Though the differential of mesalamine-induced lung injury, cannot be confirmed nor excluded here, this patient probably had underlying lung pathology from his CD or its treatment, making his recovery from COVID-19 more complicated.
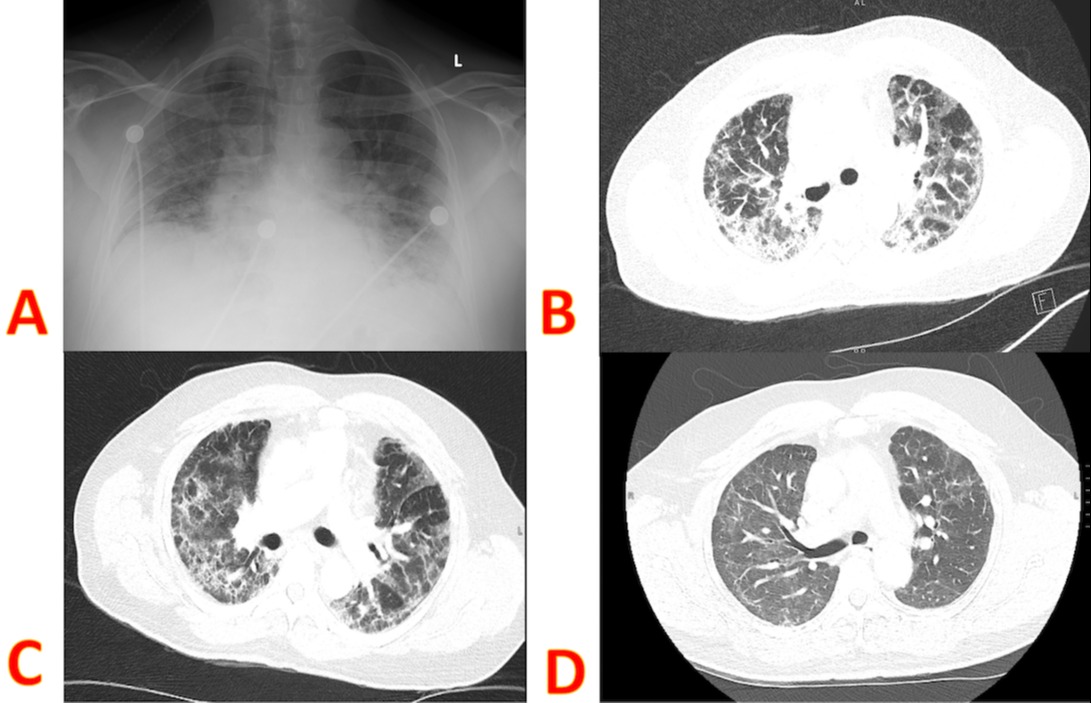
Figure: A: Portable Chest X-ray showing multifocal pneumonia, low lung volumes with bilateral patchy airspace disease; B, C: CT-Chest showing peripherally distributed ground-glass opacities, distributed in upper and lower lobes. There were superimposed early diffuse lung fibrotic changes, without any evidence of pulmonary thromboembolism; D: CT Chest, 5 months post-discharge, showing improvement in opacities.
Disclosures:
Vinay Jahagirdar indicated no relevant financial relationships.
Amulya Balagani indicated no relevant financial relationships.
Louis Saade indicated no relevant financial relationships.
Vinay Jahagirdar, MBBS1, Amulya Balagani, MBBS2, Louis Saade, MD3. C0434 - Mesalamine-Induced Interstitial Lung Disease in a Crohn’s Patient With COVID-19, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
