Back

Poster Session D - Tuesday Morning
Category: Small Intestine
D0677 - HIV/AIDS, and MAC vs COVID Diarrhea
Tuesday, October 25, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom
Has Audio
- KD
Kieu Dinh, DO
St. Rita Medical Center
Huntington, WV
Presenting Author(s)
Kieu Dinh, DO1, Rafael Nivar, MD2, Eric Kirschner, MD3, Jayde Kurland, MD4
1St. Rita Medical Center, Huntington, WV; 2Lima Memorial Health System, Lima, OH; 3St. Rita Medical Center, Lima, OH; 4Gastro Health, Lima, OH
Introduction: During the COVID pandemic, it was difficult to differentiate COVID diarrhea vs other causes, especially in the HIV/AIDS population. HIV infected patients are at high risk for GI infections. Biopsy of the small intestine identifies etiologies which help to differentiate infection, inflammatory, and neoplastic GI disease.
Case Description/Methods: A 39-year-old male presented with two months of epigastric abdominal pain, severe diarrhea, and dehydration during the COVID pandemic in 2020.
Past medical history of AIDS wasting syndrome. The patient was severely hypotensive. Exam was notable for mild epigastric tenderness,and hepatomegaly. Complete blood count (CBC) revealed a Hemoglobin (Hg) of 4.3g. Covid 19 was positive. Gastrointestinal panel PCR was negative. CD4 count 1, HIV RNA viral load 48,700. MRI of the abdomen and pelvis showed diffuse bowel wall thickening in the small intestines.
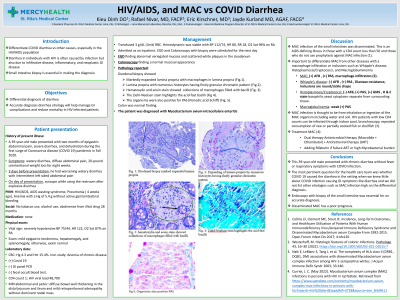
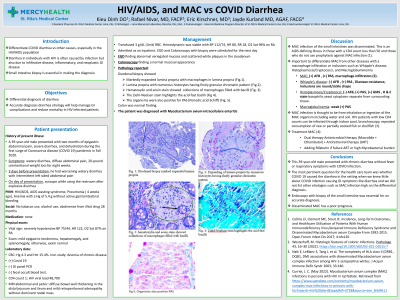
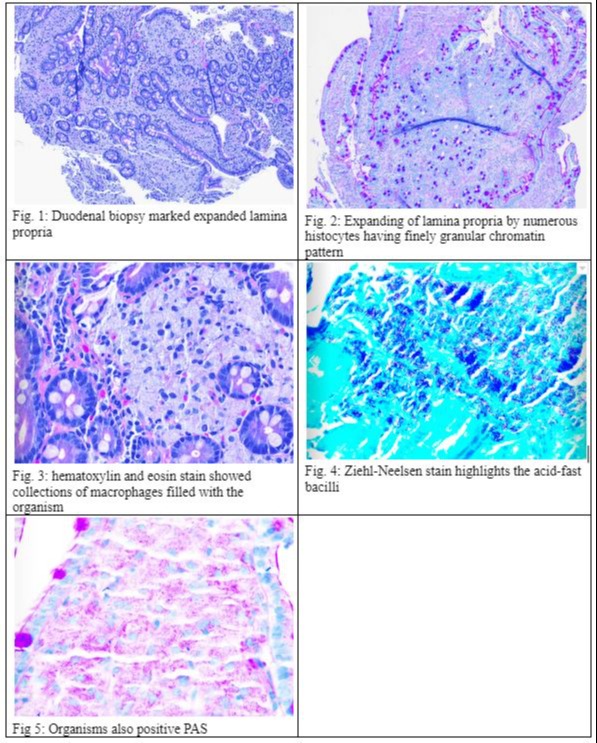
On hospital day 2, Esophagogastroduodenoscopy (EGD) and Colonoscopy were performed for anemia and diarrhea, which revealed abnormal variegated mucosa in the duodenum. Colonoscopy showed a normal mucosal appearance. The pathology report of the duodenum revealed macrophages in the lamina propria, which stained positive for Acid Fast Bacilli. Duodenal biopsy showed markedly expanded lamina propria with numerous histiocytes having finely granular chromatin pattern (Fig.1 & 2). The patient was diagnosed with Mycobacterium avium-intracellulare enteritis.
Discussion: This 39-year-old male presented with chronic diarrhea without fever or respiratory symptoms. The most pertinent question for the health care team was whether COVID 19 caused the diarrhea.. Endoscopy with biopsy of the small intestine was essential for an accurate diagnosis.
MAC infection in HIV has been dramatically declining since the widespread use of antiretroviral therapy and prophylaxis against MAC infection compared to the 1990s (from 65.3/1000 in 1992 to 2/1000 in 2015) (1).
It is important to differentiate MAC from other diseases with a macrophage infiltration or inclusions: including Whipple’s, , histoplasmosis, and macroglobulinemia. Patients with MAC enteritis present with fever, and watery diarrhea with diffuse small bowel malabsorption which mimics Whipple’s disease. However, the key to differentiate these two entities is doing a duodenal biopsy showing foamy macrophages with PAS-positive acid-fast bacilli (2).
Disclosures:
Kieu Dinh, DO1, Rafael Nivar, MD2, Eric Kirschner, MD3, Jayde Kurland, MD4. D0677 - HIV/AIDS, and MAC vs COVID Diarrhea, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1St. Rita Medical Center, Huntington, WV; 2Lima Memorial Health System, Lima, OH; 3St. Rita Medical Center, Lima, OH; 4Gastro Health, Lima, OH
Introduction: During the COVID pandemic, it was difficult to differentiate COVID diarrhea vs other causes, especially in the HIV/AIDS population. HIV infected patients are at high risk for GI infections. Biopsy of the small intestine identifies etiologies which help to differentiate infection, inflammatory, and neoplastic GI disease.
Case Description/Methods: A 39-year-old male presented with two months of epigastric abdominal pain, severe diarrhea, and dehydration during the COVID pandemic in 2020.
Past medical history of AIDS wasting syndrome. The patient was severely hypotensive. Exam was notable for mild epigastric tenderness,and hepatomegaly. Complete blood count (CBC) revealed a Hemoglobin (Hg) of 4.3g. Covid 19 was positive. Gastrointestinal panel PCR was negative. CD4 count 1, HIV RNA viral load 48,700. MRI of the abdomen and pelvis showed diffuse bowel wall thickening in the small intestines.
On hospital day 2, Esophagogastroduodenoscopy (EGD) and Colonoscopy were performed for anemia and diarrhea, which revealed abnormal variegated mucosa in the duodenum. Colonoscopy showed a normal mucosal appearance. The pathology report of the duodenum revealed macrophages in the lamina propria, which stained positive for Acid Fast Bacilli. Duodenal biopsy showed markedly expanded lamina propria with numerous histiocytes having finely granular chromatin pattern (Fig.1 & 2). The patient was diagnosed with Mycobacterium avium-intracellulare enteritis.
Discussion: This 39-year-old male presented with chronic diarrhea without fever or respiratory symptoms. The most pertinent question for the health care team was whether COVID 19 caused the diarrhea.. Endoscopy with biopsy of the small intestine was essential for an accurate diagnosis.
MAC infection in HIV has been dramatically declining since the widespread use of antiretroviral therapy and prophylaxis against MAC infection compared to the 1990s (from 65.3/1000 in 1992 to 2/1000 in 2015) (1).
It is important to differentiate MAC from other diseases with a macrophage infiltration or inclusions: including Whipple’s, , histoplasmosis, and macroglobulinemia. Patients with MAC enteritis present with fever, and watery diarrhea with diffuse small bowel malabsorption which mimics Whipple’s disease. However, the key to differentiate these two entities is doing a duodenal biopsy showing foamy macrophages with PAS-positive acid-fast bacilli (2).
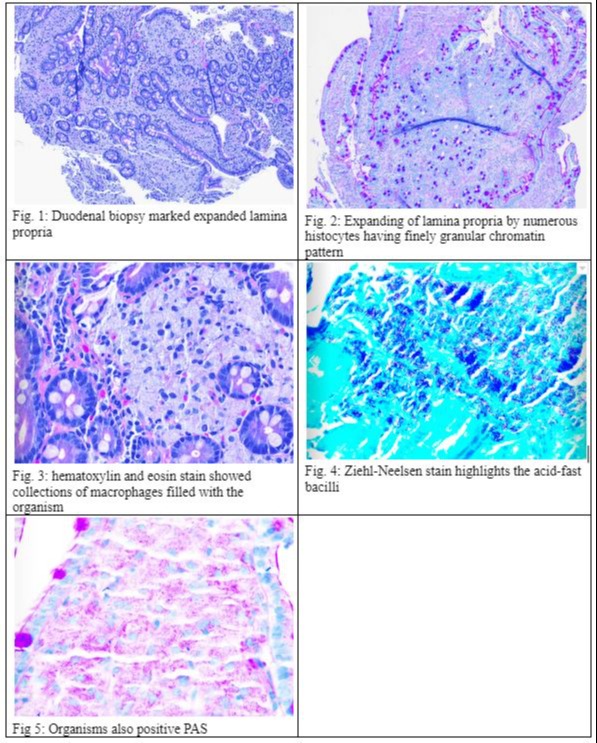
Figure: Histology finding
Disclosures:
Kieu Dinh indicated no relevant financial relationships.
Rafael Nivar indicated no relevant financial relationships.
Eric Kirschner indicated no relevant financial relationships.
Jayde Kurland indicated no relevant financial relationships.
Kieu Dinh, DO1, Rafael Nivar, MD2, Eric Kirschner, MD3, Jayde Kurland, MD4. D0677 - HIV/AIDS, and MAC vs COVID Diarrhea, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
