Back

Poster Session A - Sunday Afternoon
Category: Stomach
A0731 - Eosinophilic Gastroenteritis: A Rare Case of Unrelenting Strife
Sunday, October 23, 2022
5:00 PM – 7:00 PM ET
Location: Crown Ballroom
Has Audio
- HS
Hamza Salim, DO
University of Texas Medical Branch
Galveston, TX
Presenting Author(s)
Hamza Salim, DO1, Ernesto A. Zamora, MD1, Akshata Moghe, MBBS, PhD2
1University of Texas Medical Branch, Galveston, TX; 2University of Texas Medical Branch at Galveston, Galveston, TX
Introduction: Eosinophilic gastrointestinal diseases (EGIDs) are chronic, immune-mediated disorders characterized histologically by a pathologic increase in eosinophil-predominant tissue causing inflammation. Clinically, this group of disorders presents with chronic, non-specific gastrointestinal symptoms that can affect the entirety of the GI tract. Eosinophilic gastroenteritis specifically has a predilection for the distal antrum and proximal small bowel. In the literature, there are a small number of cases that describe eosinophilic gastroenteritis. We present a rare case of eosinophilic gastroenteritis, treated effectively with steroids leading to rapid clinical improvement.
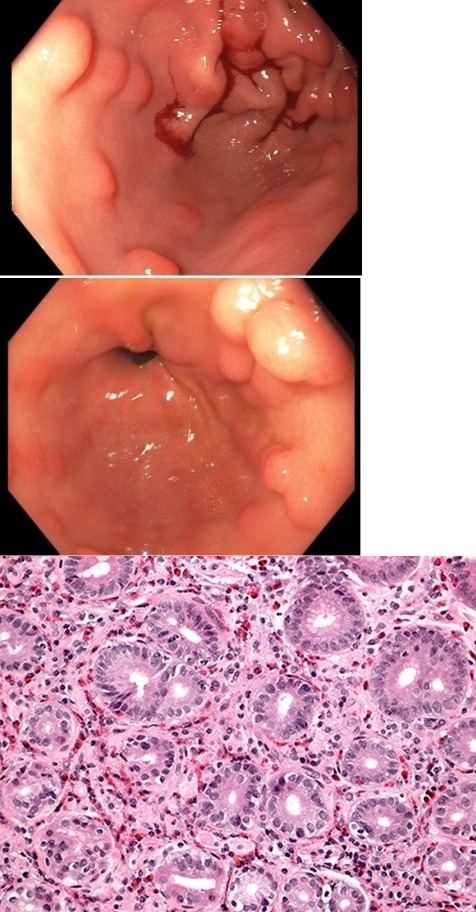
Case Description/Methods: A 45 year-old female patient with a past medical history of obesity and uncontrolled hypothyroidism presented to our institution with a five-year history of abdominal pain, nausea, and diarrhea. Prior workup showed eosinophilia but had remained unaddressed. Imaging revealed diffuse wall thickening throughout the GI tract, concerning for IBD. Extensive lab testing showed hypereosinophilia but otherwise was unremarkable. EGD revealed nodularity in the antrum with diffuse erythematous appearance. Colonoscopy was remarkable for multiple polyps in all parts of the colon. Biopsies were done and pathologic evaluation showed prominent eosinophilic infiltration in the lamina propria of the antrum and proximal small bowel. Other causes of hypereosinophilia were ruled out and our patient was diagnosed with eosinophilic gastroenteritis. She was started on a combination of steroids, a leukotriene receptor antagonist, and a mast cell stabilizer leading to improvement in symptoms with good recovery.
Discussion: The pathogenesis of eosinophilic gastrointestinal diseases is not well understood and has been studied as a hypersensitivity reaction. Infiltration of eosinophils can involve any layer of the GI tract with symptoms varying depending on depth and location of infiltration. EGIDs have been shown to persist through eosinophil-induced cytokine activation and release of eosinophil major basic protein. Therapy has not been standardized but involves steroid therapy along with various other medications and dietary modifications. Eosinophilic gastroenteritis should remain on the differential during the workup of patients with eosinophilia and GI manifestations.
Disclosures:
Hamza Salim, DO1, Ernesto A. Zamora, MD1, Akshata Moghe, MBBS, PhD2. A0731 - Eosinophilic Gastroenteritis: A Rare Case of Unrelenting Strife, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1University of Texas Medical Branch, Galveston, TX; 2University of Texas Medical Branch at Galveston, Galveston, TX
Introduction: Eosinophilic gastrointestinal diseases (EGIDs) are chronic, immune-mediated disorders characterized histologically by a pathologic increase in eosinophil-predominant tissue causing inflammation. Clinically, this group of disorders presents with chronic, non-specific gastrointestinal symptoms that can affect the entirety of the GI tract. Eosinophilic gastroenteritis specifically has a predilection for the distal antrum and proximal small bowel. In the literature, there are a small number of cases that describe eosinophilic gastroenteritis. We present a rare case of eosinophilic gastroenteritis, treated effectively with steroids leading to rapid clinical improvement.
Case Description/Methods: A 45 year-old female patient with a past medical history of obesity and uncontrolled hypothyroidism presented to our institution with a five-year history of abdominal pain, nausea, and diarrhea. Prior workup showed eosinophilia but had remained unaddressed. Imaging revealed diffuse wall thickening throughout the GI tract, concerning for IBD. Extensive lab testing showed hypereosinophilia but otherwise was unremarkable. EGD revealed nodularity in the antrum with diffuse erythematous appearance. Colonoscopy was remarkable for multiple polyps in all parts of the colon. Biopsies were done and pathologic evaluation showed prominent eosinophilic infiltration in the lamina propria of the antrum and proximal small bowel. Other causes of hypereosinophilia were ruled out and our patient was diagnosed with eosinophilic gastroenteritis. She was started on a combination of steroids, a leukotriene receptor antagonist, and a mast cell stabilizer leading to improvement in symptoms with good recovery.
Discussion: The pathogenesis of eosinophilic gastrointestinal diseases is not well understood and has been studied as a hypersensitivity reaction. Infiltration of eosinophils can involve any layer of the GI tract with symptoms varying depending on depth and location of infiltration. EGIDs have been shown to persist through eosinophil-induced cytokine activation and release of eosinophil major basic protein. Therapy has not been standardized but involves steroid therapy along with various other medications and dietary modifications. Eosinophilic gastroenteritis should remain on the differential during the workup of patients with eosinophilia and GI manifestations.
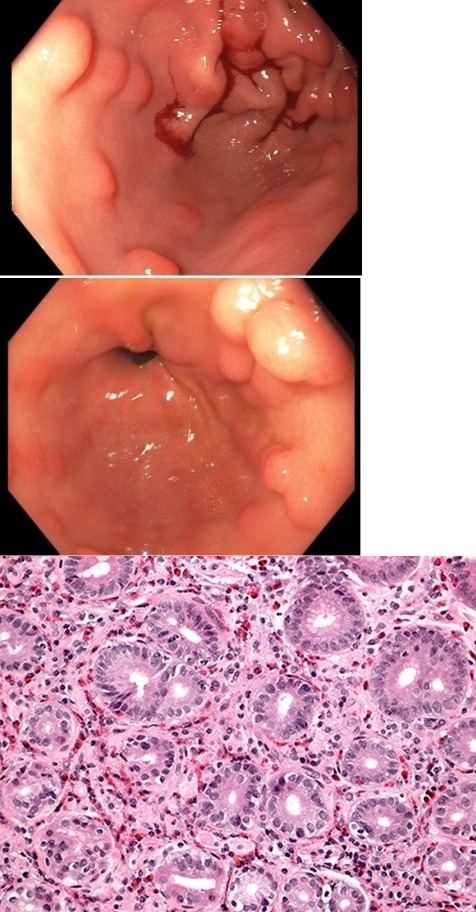
Figure: Figure 1: Nodular appearance of the antrum with active oozing seen after biopsy.
Figure 2: Pyloric view showing continued nodularity, consistent with eosinophilic gastritis.
Figure 3: Hematoxylin and eosin staining showing eosinophilic infiltration of the lamina propria.
Figure 2: Pyloric view showing continued nodularity, consistent with eosinophilic gastritis.
Figure 3: Hematoxylin and eosin staining showing eosinophilic infiltration of the lamina propria.
Disclosures:
Hamza Salim indicated no relevant financial relationships.
Ernesto Zamora indicated no relevant financial relationships.
Akshata Moghe indicated no relevant financial relationships.
Hamza Salim, DO1, Ernesto A. Zamora, MD1, Akshata Moghe, MBBS, PhD2. A0731 - Eosinophilic Gastroenteritis: A Rare Case of Unrelenting Strife, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
