Back


Poster Session C - Monday Afternoon
Category: GI Bleeding
C0355 - The Unusual Suspect: Gastrointestinal Bleeding From an Ampullary Dieulafoy Lesion
Monday, October 24, 2022
3:00 PM – 5:00 PM ET
Location: Crown Ballroom

Has Audio

Syed Hamza Sohail, MD
UMass Chan - Baystate Medical Center
Springfield, MA
Presenting Author(s)
Syed Hamza Sohail, MD1, Bushra Zia, MD2, Kevin Groudan, MD3, David Desilets, MD3
1UMass Chan - Baystate Medical Center, Springfield, MA; 2UMass Chan Medical School - Baystate, Springfield, MA; 3University of Massachusetts Medical School - Baystate, Springfield, MA
Introduction: Dieulafoy lesions (DLs) are an unusual but important cause of acute upper gastrointestinal bleeding (UGIBs), and can be difficult to diagnose. Three fourths are found in the stomach close to the gastroesophageal junction, but have also been reported in small bowel and colon. There are only a few reported cases of ampullary DLs. We present a rare case of a recurrent UGIB from an ampullary Dieulafoy lesion and its management.
Case Description/Methods: A 65-year-old male presented for type B aortic dissection requiring endovascular repair, which was complicated by type 1 endoleak. His hospital course was complex owing to sepsis, respiratory failure, and cardiac arrest. Gastroenterology was consulted on day 16 for multiple tarry bowel movements.
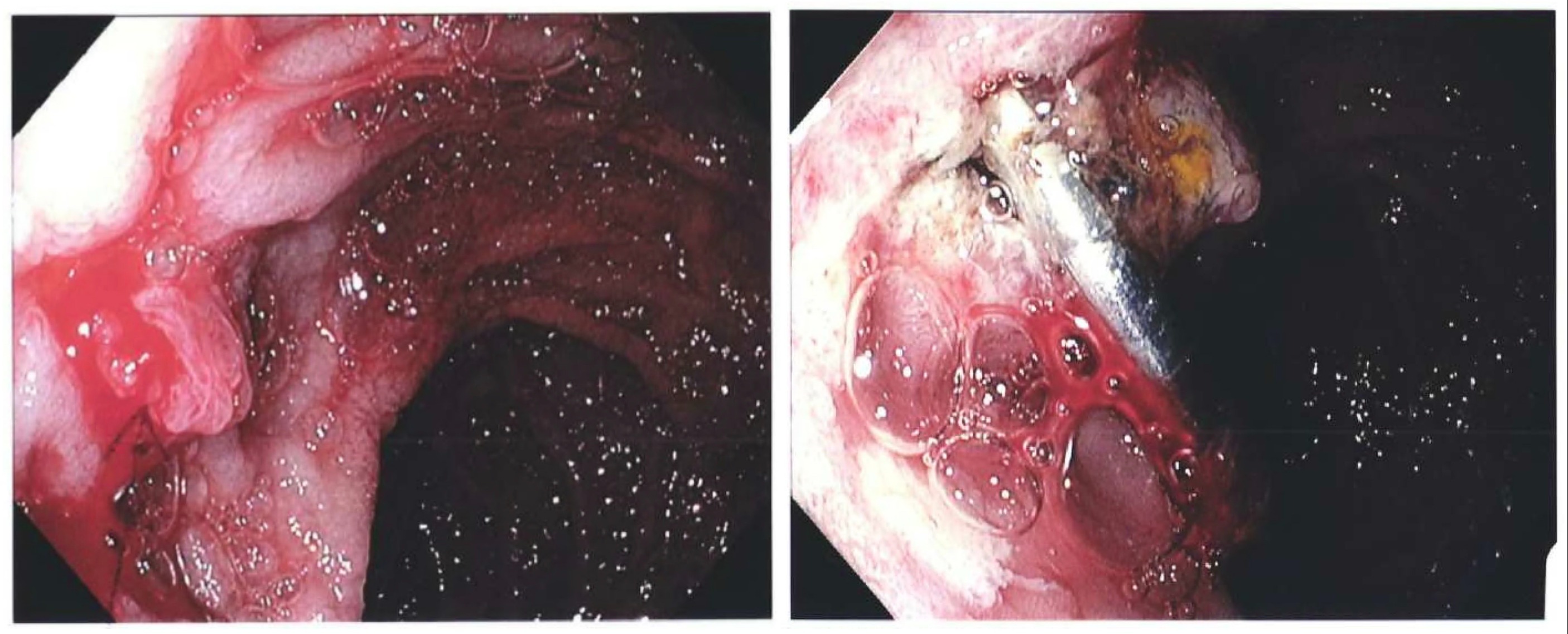
Esophagogastroduodenoscopy (EGD) showed healing ulcers in lower esophagus. and non-bleeding ulcers in the duodenal bulb. The culprit lesion was an oozing Dieulafoy at the major papilla. Hemostasis was achieved with epinephrine injection and thermal therapy.
Rebleeding occurred 5 days after the initial EGD leading to shock and cardiac arrest. Once the patient was hemodynamically stabilized, he underwent another EGD that showed copious fresh blood in stomach body as well as the second and third portions of duodenum. Active arterial spurting was noted from the superior aspect of major papilla.
Given the severe hemodynamic compromise from this bleeding, we elected to clip the lesion this time, accepting the risk of pancreatitis and/or biliary obstruction. One endoclip was placed across the dorsal aspect of major papilla and closed. Persistent oozing was noted from under the clip which was arrested by applying a hot snare to the already placed endoclip and delivering thermal energy to the area pinched by the endoclip. Complete hemostasis was then achieved. [Figure 1]
Liver function tests and lipase were monitored for a week and the patient did not develop pancreatitis or biliary obstruction despite placement of endoclip across the major papilla.
Discussion: Ampullary DLs are extremely rare and can present a unique diagnostic and therapeutic challenge due to their anatomical location. There is currently no consensus on how to best treat ampullary DLs. Verification of the diagnosis and definitive treatment might require repeated examinations. Early and aggressive endoscopic treatment should be adopted when an ampullary DL is suspected, and patients should be closely followed up given therapeutic interventions can potentially impair biliary drainage.
Disclosures:
Syed Hamza Sohail, MD1, Bushra Zia, MD2, Kevin Groudan, MD3, David Desilets, MD3. C0355 - The Unusual Suspect: Gastrointestinal Bleeding From an Ampullary Dieulafoy Lesion, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1UMass Chan - Baystate Medical Center, Springfield, MA; 2UMass Chan Medical School - Baystate, Springfield, MA; 3University of Massachusetts Medical School - Baystate, Springfield, MA
Introduction: Dieulafoy lesions (DLs) are an unusual but important cause of acute upper gastrointestinal bleeding (UGIBs), and can be difficult to diagnose. Three fourths are found in the stomach close to the gastroesophageal junction, but have also been reported in small bowel and colon. There are only a few reported cases of ampullary DLs. We present a rare case of a recurrent UGIB from an ampullary Dieulafoy lesion and its management.
Case Description/Methods: A 65-year-old male presented for type B aortic dissection requiring endovascular repair, which was complicated by type 1 endoleak. His hospital course was complex owing to sepsis, respiratory failure, and cardiac arrest. Gastroenterology was consulted on day 16 for multiple tarry bowel movements.
Esophagogastroduodenoscopy (EGD) showed healing ulcers in lower esophagus. and non-bleeding ulcers in the duodenal bulb. The culprit lesion was an oozing Dieulafoy at the major papilla. Hemostasis was achieved with epinephrine injection and thermal therapy.
Rebleeding occurred 5 days after the initial EGD leading to shock and cardiac arrest. Once the patient was hemodynamically stabilized, he underwent another EGD that showed copious fresh blood in stomach body as well as the second and third portions of duodenum. Active arterial spurting was noted from the superior aspect of major papilla.
Given the severe hemodynamic compromise from this bleeding, we elected to clip the lesion this time, accepting the risk of pancreatitis and/or biliary obstruction. One endoclip was placed across the dorsal aspect of major papilla and closed. Persistent oozing was noted from under the clip which was arrested by applying a hot snare to the already placed endoclip and delivering thermal energy to the area pinched by the endoclip. Complete hemostasis was then achieved. [Figure 1]
Liver function tests and lipase were monitored for a week and the patient did not develop pancreatitis or biliary obstruction despite placement of endoclip across the major papilla.
Discussion: Ampullary DLs are extremely rare and can present a unique diagnostic and therapeutic challenge due to their anatomical location. There is currently no consensus on how to best treat ampullary DLs. Verification of the diagnosis and definitive treatment might require repeated examinations. Early and aggressive endoscopic treatment should be adopted when an ampullary DL is suspected, and patients should be closely followed up given therapeutic interventions can potentially impair biliary drainage.
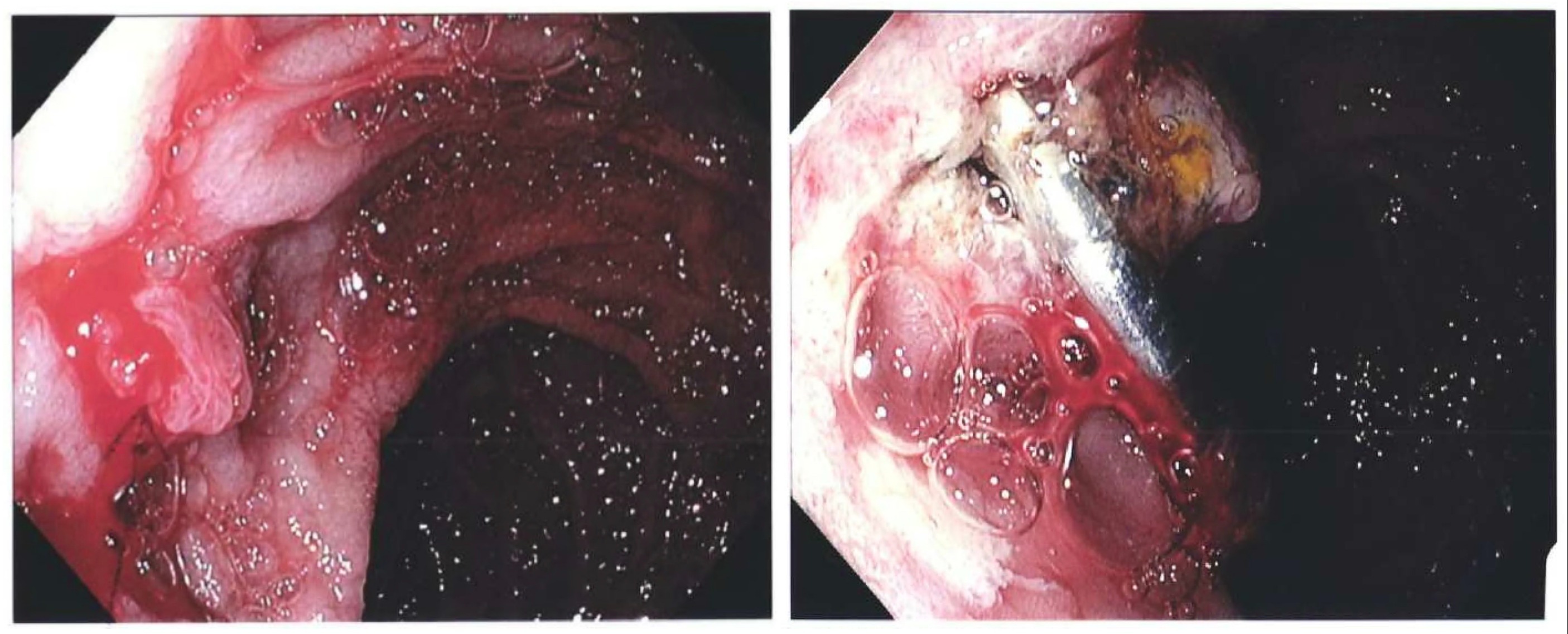
Figure: Figure 1: Endoscopic images of bleeding from ampullary Dieulafoy lesion before and after endoscopic intervention.
Disclosures:
Syed Hamza Sohail indicated no relevant financial relationships.
Bushra Zia indicated no relevant financial relationships.
Kevin Groudan indicated no relevant financial relationships.
David Desilets indicated no relevant financial relationships.
Syed Hamza Sohail, MD1, Bushra Zia, MD2, Kevin Groudan, MD3, David Desilets, MD3. C0355 - The Unusual Suspect: Gastrointestinal Bleeding From an Ampullary Dieulafoy Lesion, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
