Back

Poster Session D - Tuesday Morning
Category: Stomach
D0724 - An Uncommon Pulsating Submucosal Gastric Lesion
Tuesday, October 25, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom
Has Audio

Kevin Kadado, DO
University of Kansas
Wichita, KS
Presenting Author(s)
Kevin Kadado, DO1, Estephan Zayat, MD2, Bassem Matta, MD3
1University of Kansas, Wichita, KS; 2University of Kansas School of Medicine, Wichita, KS; 3Kansas Gastroenterology, Wichita, KS
Introduction: Gastric hamartomatous inverted polyps (GHIP) are extremely rare submucosal lesions. These polyps are commonly asymptomatic and are found incidentally during esophagogastroduodenoscopy (EGD). While gastric polyps are benign in nature, 20% of GHIP possess foci of gastric adenocarcinoma. As such, en-bloc endoscopic or surgical resection is the treatment of choice. We describe a challenging case of a large GHIP in the setting of esophageal stenosis secondary to eosinophilic esophagitis (EOE).
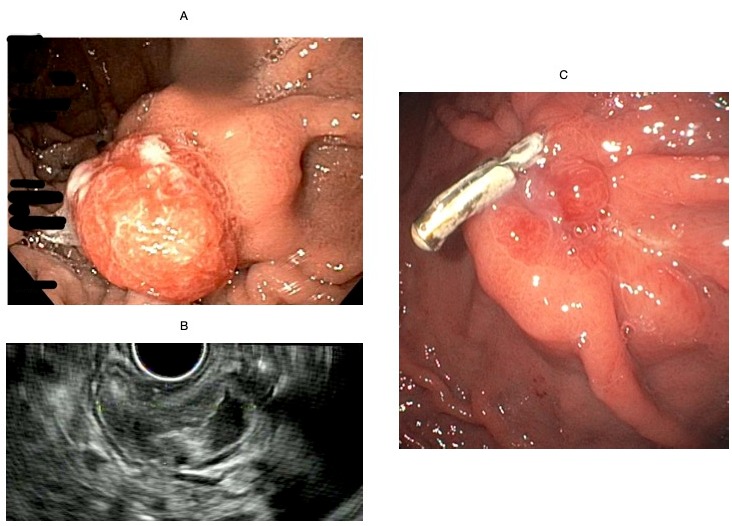
Case Description/Methods: A 40-year-old male with no significant past medical history was referred to our clinic for dysphagia. EGD at this time was significant for severe esophageal stenosis with circular rings consistent with EOE and a 3 cm pulsating, polypoid submucosal mass at the gastric fundus (Figure A). Given the pulsatile nature of the mass, biopsy was deferred. Computed Tomography of the abdomen with contrast was significant for a 2.1 cm gastric wall mass, suspicious for a gastrointestinal stromal tumor (GIST). Endoscopic ultrasound (EUS), after esophageal dilation, was performed revealing a 25 x 15 mm submucosal gastric mass in the fundus, originating from the muscularis mucosa (Figure B). Fine needle biopsy (FNBx) was considered benign but inconclusive due to blood. The pathologist recommended additional tissue. An EGD was later performed with piecemeal endoscopic mucosal resection (EMR) followed by clip closure at the resection site. An endoscopic submucosal dissection (ESD) was not undertaken in this situation due to severe esophageal stenosis and inability to advance a scope with a distal attachment cap through the narrow esophagus. The final pathology was consistent with a GHIP. Follow up endoscopy revealed no residual tissue (Figure C). After discussion with the patient and due the risk of malignancy and inability to guarantee negative margins on a piecemeal resection, he was given the option of endoscopic surveillance vs. surgical resection, he elected the latter option. Robotic wedge gastrectomy was performed and revealed no residual GHIP.
Discussion: GHIP is a rare lesion often mistaken for GIST. After histological diagnosis, the treatment of choice for GHIP is en-bloc resection. This presentation with esophageal stenosis due to EOE made it extremely challenging to follow these traditional approaches. This case highlights how endoscopic mucosal resection can be used to resect these types of lesions.
Disclosures:
Kevin Kadado, DO1, Estephan Zayat, MD2, Bassem Matta, MD3. D0724 - An Uncommon Pulsating Submucosal Gastric Lesion, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1University of Kansas, Wichita, KS; 2University of Kansas School of Medicine, Wichita, KS; 3Kansas Gastroenterology, Wichita, KS
Introduction: Gastric hamartomatous inverted polyps (GHIP) are extremely rare submucosal lesions. These polyps are commonly asymptomatic and are found incidentally during esophagogastroduodenoscopy (EGD). While gastric polyps are benign in nature, 20% of GHIP possess foci of gastric adenocarcinoma. As such, en-bloc endoscopic or surgical resection is the treatment of choice. We describe a challenging case of a large GHIP in the setting of esophageal stenosis secondary to eosinophilic esophagitis (EOE).
Case Description/Methods: A 40-year-old male with no significant past medical history was referred to our clinic for dysphagia. EGD at this time was significant for severe esophageal stenosis with circular rings consistent with EOE and a 3 cm pulsating, polypoid submucosal mass at the gastric fundus (Figure A). Given the pulsatile nature of the mass, biopsy was deferred. Computed Tomography of the abdomen with contrast was significant for a 2.1 cm gastric wall mass, suspicious for a gastrointestinal stromal tumor (GIST). Endoscopic ultrasound (EUS), after esophageal dilation, was performed revealing a 25 x 15 mm submucosal gastric mass in the fundus, originating from the muscularis mucosa (Figure B). Fine needle biopsy (FNBx) was considered benign but inconclusive due to blood. The pathologist recommended additional tissue. An EGD was later performed with piecemeal endoscopic mucosal resection (EMR) followed by clip closure at the resection site. An endoscopic submucosal dissection (ESD) was not undertaken in this situation due to severe esophageal stenosis and inability to advance a scope with a distal attachment cap through the narrow esophagus. The final pathology was consistent with a GHIP. Follow up endoscopy revealed no residual tissue (Figure C). After discussion with the patient and due the risk of malignancy and inability to guarantee negative margins on a piecemeal resection, he was given the option of endoscopic surveillance vs. surgical resection, he elected the latter option. Robotic wedge gastrectomy was performed and revealed no residual GHIP.
Discussion: GHIP is a rare lesion often mistaken for GIST. After histological diagnosis, the treatment of choice for GHIP is en-bloc resection. This presentation with esophageal stenosis due to EOE made it extremely challenging to follow these traditional approaches. This case highlights how endoscopic mucosal resection can be used to resect these types of lesions.
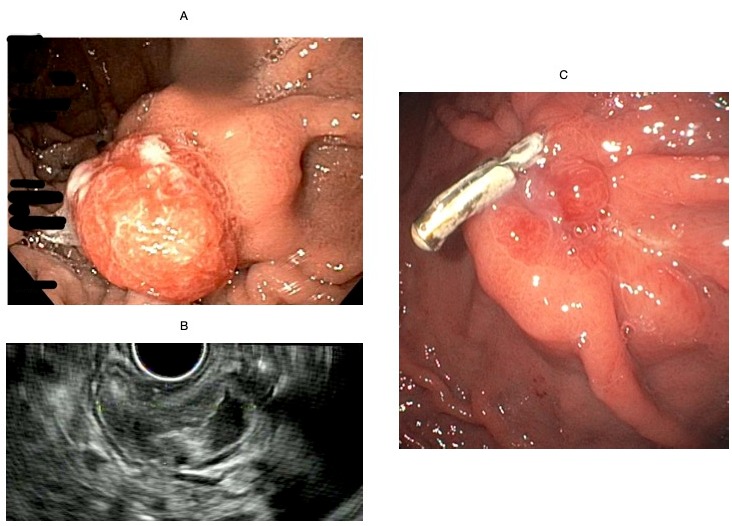
Figure: Figure A - Pulsating submucosal gastric fundus lesion seen on EGD ; Figure B - EUS image of the submucosal lesion ; Figure C - Resection scar at follow up EGD with granulation tissue and retained clip
Disclosures:
Kevin Kadado indicated no relevant financial relationships.
Estephan Zayat indicated no relevant financial relationships.
Bassem Matta indicated no relevant financial relationships.
Kevin Kadado, DO1, Estephan Zayat, MD2, Bassem Matta, MD3. D0724 - An Uncommon Pulsating Submucosal Gastric Lesion, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
