Back

Poster Session D - Tuesday Morning
Category: Esophagus
D0256 - Esophageal Stricture Secondary to Mycophenolate Mofetil-Induced Injury
Tuesday, October 25, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom
Has Audio

Nicole L. Miller, MD
University of South Florida Morsani College of Medicine
Tampa, FL
Presenting Author(s)
Nicole L. Miller, MD1, Brian Frank, MD2, John Jacobs, MD3
1University of South Florida Morsani College of Medicine, Tampa, FL; 2University of South Florida, Tampa, FL; 3University of South Florida Health, Tampa, FL
Introduction: Immunosuppressant medications like mycophenolate mofetil (MMF) have recently garnered more attention in the literature due to gastrointestinal toxicity. There are increasing case reports of transplant patients on MMF who develop inflammation or ulcers throughout the GI tract. It is theorized that the inflammation is due to MMF toxicity from metabolite formation. Although there has been increasing evidence of MMF induced injury to the GI tract, there are few reports of esophageal involvement, which is presented below.
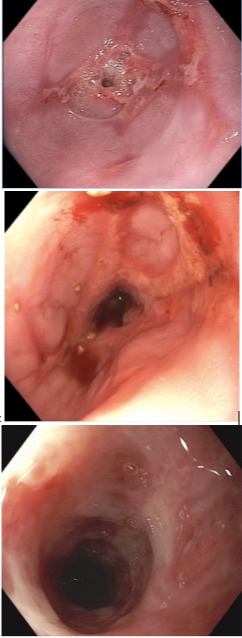
Case Description/Methods: This case involves a 40 year-old patient with Type I diabetes mellitus complicated by gastroparesis, renal and pancreatic transplants on immunosuppression with MMF, who developed progressively worsening dysphagia, weight loss, nausea, and vomiting. The patient initially presented to an outside gastroenterologist due to complaints of nausea and hematemesis. An EGD was completed with evidence of ulcerative esophagitis with biopsies negative for bacterial, fungal and viral stains. He was started on a proton pump inhibitor (PPI) for treatment of presumed reflux esophagitis. After no improvement with several months of therapy, he presented to our gastroenterology clinic for evaluation. Upon questioning, he specifically complained of progressive difficulty with swallowing after starting MMF. The patient underwent EGD and showed a severe distal esophageal stricture, which was not able to be traversed with the regular upper endoscope [figure 1]. Biopsies were taken and revealed acute erosive esophagitis. Immunohistochemical staining was negative for HSV and CMV. Given our high suspicion for MMF-induced esophageal injury, his medication was changed to liquid formulation. The patient underwent repeat serial endoscopies with dilation every 2 weeks for the next 2 months. After transitioning to liquid formulation, each subsequent endoscopy showed improvement in the ulcerated stricture. The patient was last dilated to 45 French in which he reported marked improvement of his dysphagia.
Discussion: This case demonstrates a patient who developed a severe esophageal stricture from MMF induced injury with resolution of symptoms after multiple dilations and transition to a liquid formulation of MMF. Though the exact physiologic mechanisms are not well understood, gastroenterologists should be suspicious in patients on mycophenolate who present with dysphagia and stricture that is not explained by infection, malignancy, reflux, or other medications.
Disclosures:
Nicole L. Miller, MD1, Brian Frank, MD2, John Jacobs, MD3. D0256 - Esophageal Stricture Secondary to Mycophenolate Mofetil-Induced Injury, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1University of South Florida Morsani College of Medicine, Tampa, FL; 2University of South Florida, Tampa, FL; 3University of South Florida Health, Tampa, FL
Introduction: Immunosuppressant medications like mycophenolate mofetil (MMF) have recently garnered more attention in the literature due to gastrointestinal toxicity. There are increasing case reports of transplant patients on MMF who develop inflammation or ulcers throughout the GI tract. It is theorized that the inflammation is due to MMF toxicity from metabolite formation. Although there has been increasing evidence of MMF induced injury to the GI tract, there are few reports of esophageal involvement, which is presented below.
Case Description/Methods: This case involves a 40 year-old patient with Type I diabetes mellitus complicated by gastroparesis, renal and pancreatic transplants on immunosuppression with MMF, who developed progressively worsening dysphagia, weight loss, nausea, and vomiting. The patient initially presented to an outside gastroenterologist due to complaints of nausea and hematemesis. An EGD was completed with evidence of ulcerative esophagitis with biopsies negative for bacterial, fungal and viral stains. He was started on a proton pump inhibitor (PPI) for treatment of presumed reflux esophagitis. After no improvement with several months of therapy, he presented to our gastroenterology clinic for evaluation. Upon questioning, he specifically complained of progressive difficulty with swallowing after starting MMF. The patient underwent EGD and showed a severe distal esophageal stricture, which was not able to be traversed with the regular upper endoscope [figure 1]. Biopsies were taken and revealed acute erosive esophagitis. Immunohistochemical staining was negative for HSV and CMV. Given our high suspicion for MMF-induced esophageal injury, his medication was changed to liquid formulation. The patient underwent repeat serial endoscopies with dilation every 2 weeks for the next 2 months. After transitioning to liquid formulation, each subsequent endoscopy showed improvement in the ulcerated stricture. The patient was last dilated to 45 French in which he reported marked improvement of his dysphagia.
Discussion: This case demonstrates a patient who developed a severe esophageal stricture from MMF induced injury with resolution of symptoms after multiple dilations and transition to a liquid formulation of MMF. Though the exact physiologic mechanisms are not well understood, gastroenterologists should be suspicious in patients on mycophenolate who present with dysphagia and stricture that is not explained by infection, malignancy, reflux, or other medications.
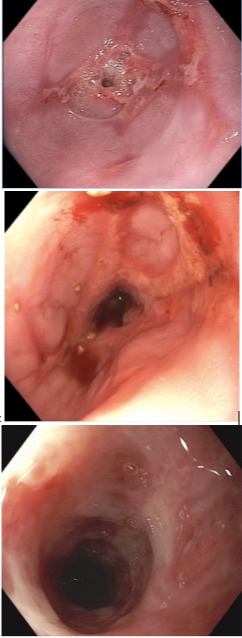
Figure: A. Initial non-traversable esophageal stricture
B. Esophageal stricture status post multiple dilations
C. Improving ulcerative stricture after switching to liquid formulation of MMF and multiple dilations
B. Esophageal stricture status post multiple dilations
C. Improving ulcerative stricture after switching to liquid formulation of MMF and multiple dilations
Disclosures:
Nicole Miller indicated no relevant financial relationships.
Brian Frank indicated no relevant financial relationships.
John Jacobs indicated no relevant financial relationships.
Nicole L. Miller, MD1, Brian Frank, MD2, John Jacobs, MD3. D0256 - Esophageal Stricture Secondary to Mycophenolate Mofetil-Induced Injury, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
