Back

Poster Session E - Tuesday Afternoon
Category: Endoscopy Video Forum
E0185 - Cystic Artery Pseudoaneurysm: A Rare Case of Upper Gastrointestinal Bleeding
Tuesday, October 25, 2022
3:00 PM – 5:00 PM ET
Location: Crown Ballroom
Has Audio
- CT
Chin Kimg Tan, MD
Changi General Hospital
Singapore, Singapore
Presenting Author(s)
Chin Kimg Tan, MD, Nita Thiruchelvam, MBBS, Kenneth Weicong Lin, MBBS, Tiing Leong Ang, MBBS
Changi General Hospital, Singapore, Singapore
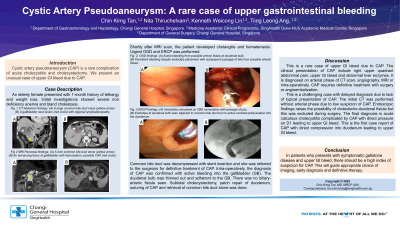
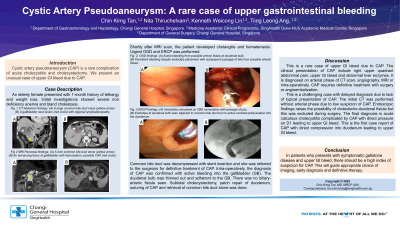
Introduction: Cystic artery pseudoaneurysm (CAP) is a rare complication of acute cholecystitis and cholecystectomy. We present an unusual case of upper GI bleed due to CAP.
Case Description/Methods: An elderly female presented with one month history of lethargy and unintentional weight loss. Clinical exam was unremarkable apart from pallor. Blood tests revealed severe iron deficiency anaemia and bland cholestasis. CT scan showed a common bile duct (CBD) mass and a gallbladder (GB) neck lesion with prominent regional lymph nodes, which was worrying for biliary malignancy. MRI scan showed a 3cm CBD stone with acute emphysematous cholecystitis and possible CAP at the GB neck. An urgent OGD and ERCP was done on the same day as she developed hematemesis and cholangitis. On endoscopy, there was active bleeding from possible enteric fistula at first part of duodenum (D1), this was treated with metal clips. During ERCP, haemobilia was noted on CBD cannulation. On cholangiogram, the endoclips were adjacent to distal CBD stone. A plastic stent was inserted into the CBD and she was referred to the surgeons. Cholecystectomy and CBD exploration was performed for definitive treatment. Intra-operatively, there was active bleeding into the GB from CAP. D1 was thinned out with adhesions to the GB. There was stale blood in the bile duct but no biliary-enteric fistula seen. CAP was sutured, adhesiolysis, subtotal cholecystectomy, omental patch repair of D1 and CBD stone was retrieved. Repeat OGD and ERCP with CBD stent removal done 2 months later showed healed D1 mucosa.
Discussion: The clinical features of CAP include right upper quadrant pain, upper GI bleed due to haemobilia and abnormal liver enzymes. It is diagnosed on arterial phase of CT scan, angiography, MRI or during surgery. It is treated with surgery or angioembolization. This is a challenging case with delayed diagnosis of CAP as she lacks the typical presentation of CAP. A plain contrasted CT without arterial phase was done initially, which have mistaken the CAP as soft tissue lesion in GB. Endoscopic findings raises possibility of choledocho-duodenal fistula; this was excluded during surgery. The final diagnosis is acute calculous cholecystitis complicated by CAP with direct pressure on D1 leading to upper GI bleed. To our knowledge, this is the first case of CAP with such entity.
In conclusion, CAP should be considered in patients with symptomatic gallstone disease and upper GI bleed in order to select appropriate imaging modality and guide therapy.
Disclosures:
Chin Kimg Tan, MD, Nita Thiruchelvam, MBBS, Kenneth Weicong Lin, MBBS, Tiing Leong Ang, MBBS. E0185 - Cystic Artery Pseudoaneurysm: A Rare Case of Upper Gastrointestinal Bleeding, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
Changi General Hospital, Singapore, Singapore
Introduction: Cystic artery pseudoaneurysm (CAP) is a rare complication of acute cholecystitis and cholecystectomy. We present an unusual case of upper GI bleed due to CAP.
Case Description/Methods: An elderly female presented with one month history of lethargy and unintentional weight loss. Clinical exam was unremarkable apart from pallor. Blood tests revealed severe iron deficiency anaemia and bland cholestasis. CT scan showed a common bile duct (CBD) mass and a gallbladder (GB) neck lesion with prominent regional lymph nodes, which was worrying for biliary malignancy. MRI scan showed a 3cm CBD stone with acute emphysematous cholecystitis and possible CAP at the GB neck. An urgent OGD and ERCP was done on the same day as she developed hematemesis and cholangitis. On endoscopy, there was active bleeding from possible enteric fistula at first part of duodenum (D1), this was treated with metal clips. During ERCP, haemobilia was noted on CBD cannulation. On cholangiogram, the endoclips were adjacent to distal CBD stone. A plastic stent was inserted into the CBD and she was referred to the surgeons. Cholecystectomy and CBD exploration was performed for definitive treatment. Intra-operatively, there was active bleeding into the GB from CAP. D1 was thinned out with adhesions to the GB. There was stale blood in the bile duct but no biliary-enteric fistula seen. CAP was sutured, adhesiolysis, subtotal cholecystectomy, omental patch repair of D1 and CBD stone was retrieved. Repeat OGD and ERCP with CBD stent removal done 2 months later showed healed D1 mucosa.
Discussion: The clinical features of CAP include right upper quadrant pain, upper GI bleed due to haemobilia and abnormal liver enzymes. It is diagnosed on arterial phase of CT scan, angiography, MRI or during surgery. It is treated with surgery or angioembolization. This is a challenging case with delayed diagnosis of CAP as she lacks the typical presentation of CAP. A plain contrasted CT without arterial phase was done initially, which have mistaken the CAP as soft tissue lesion in GB. Endoscopic findings raises possibility of choledocho-duodenal fistula; this was excluded during surgery. The final diagnosis is acute calculous cholecystitis complicated by CAP with direct pressure on D1 leading to upper GI bleed. To our knowledge, this is the first case of CAP with such entity.
In conclusion, CAP should be considered in patients with symptomatic gallstone disease and upper GI bleed in order to select appropriate imaging modality and guide therapy.
Disclosures:
Chin Kimg Tan indicated no relevant financial relationships.
Nita Thiruchelvam indicated no relevant financial relationships.
Kenneth Weicong Lin indicated no relevant financial relationships.
Tiing Leong Ang indicated no relevant financial relationships.
Chin Kimg Tan, MD, Nita Thiruchelvam, MBBS, Kenneth Weicong Lin, MBBS, Tiing Leong Ang, MBBS. E0185 - Cystic Artery Pseudoaneurysm: A Rare Case of Upper Gastrointestinal Bleeding, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
