Back

Poster Session E - Tuesday Afternoon
Category: Esophagus
E0196 - The Impact of Centralized Care in the Management of Barrett’s Related Neoplasia: A Systematic Review and Meta-Analysis
Tuesday, October 25, 2022
3:00 PM – 5:00 PM ET
Location: Crown Ballroom
Has Audio

Christian Davis, MD
University of Colorado, Anschutz Medical Center
Aurora, CO
Presenting Author(s)
Award: Presidential Poster Award
Christian Davis, MD1, Andrew Fuller, MD2, David A. Katzka, MD3, Sachin Wani, MD1, Tarek Sawas, MD, MPH2
1University of Colorado, Anschutz Medical Center, Aurora, CO; 2University of Texas Southwestern, Dallas, TX; 3Columbia University, New York, NY
Introduction: Endoscopic eradication therapy (EET) is well-established for management of Barrett’s esophagus (BE) related neoplasia and increasingly being performed at tertiary care and community centers. While it has been suggested that these patients should be evaluated at expert centers, the impact of this practice has not been evaluated. We aimed to assess the impact of referral of BE-related neoplasia patients to expert centers by performing a systematic review and a meta-analysis and assessing the proportion of patients with change in pathologic diagnosis and visible lesions detected.
Methods: We searched multiple databases from inception until December 2021 for studies of patients with BE found in the community and referred to an expert center. Studies were included if they reported endoscopic and/or histologic findings in the community and after referral to an expert center. Studies were excluded if conducted in one setting only, insufficient data to determine the number of new visible lesions or pathology grade and studies with fewer than 10 subjects. The proportions of newly detected visible lesions and pathology grade change were pooled and weighted using a random effects model.
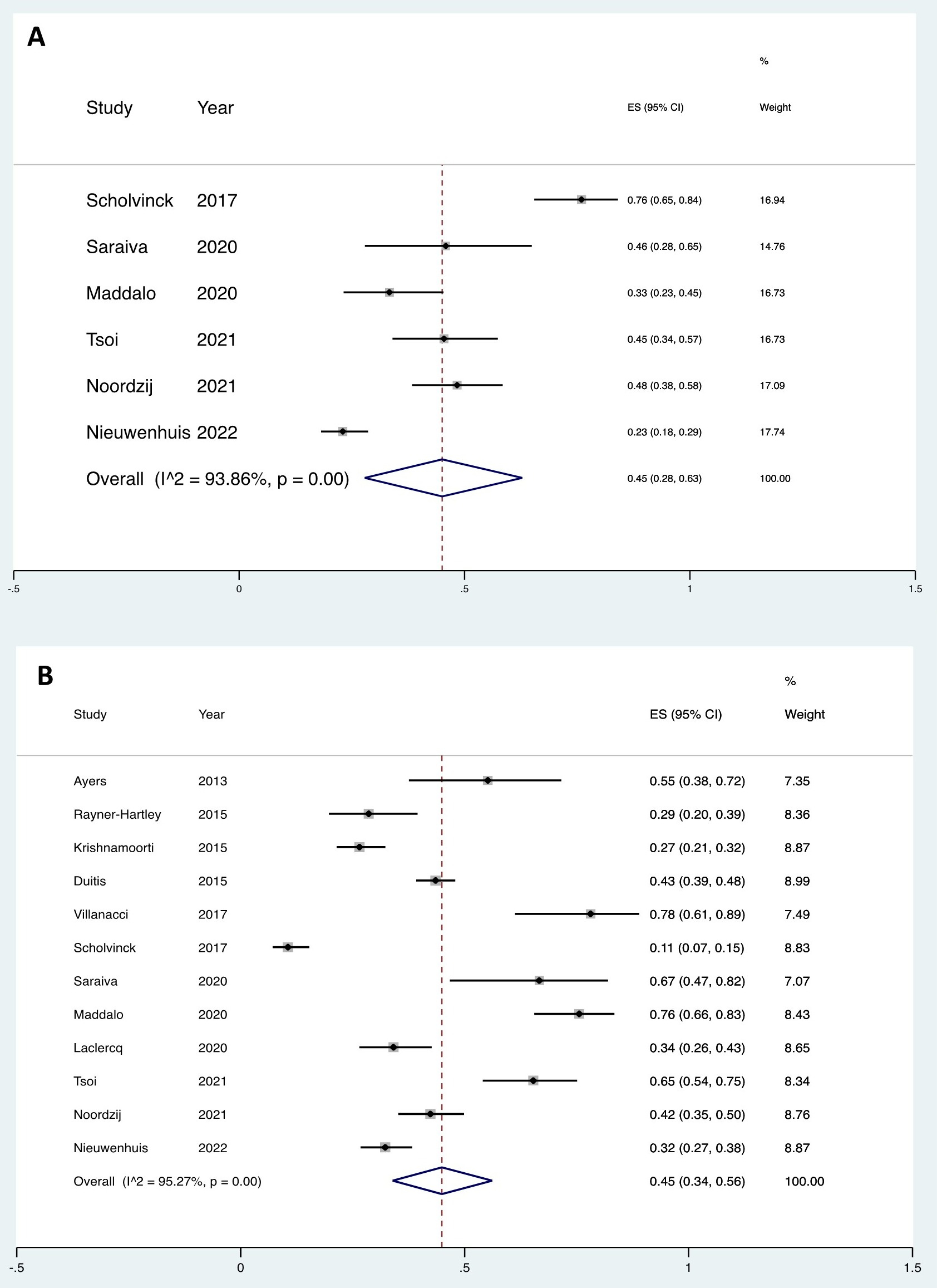
Results: Twelve studies met inclusion criteria that included 1829 patients. The pooled proportion of newly detected visible lesions was 45% (95% CI: 28%-63%, I2: 93.9%) (Figure A). The pooled proportion of pathology grade change when reviewed at an expert center was 45% (95% CI: 34%-56%, I2: 95.3%) (Figure B). The pooled proportion of pathology grade change after the endoscopy was repeated at an expert center was 47% (95%: 26% - 69%, I2: 97.2%). Patients referred with low-grade dysplasia (LGD) to expert centers had a pooled proportion of newly detectable visible lesions of 27% (95% CI: 22% - 32%, I2: 0%). The pooled proportion of pathologic grade change in patients referred with LGD when reviewed by an expert GI pathologist was 59% (95% CI: 40% - 77%, I2: 96.3%) and after repeat endoscopy was 40% (95% CI: 34% - 45%).
Discussion: An alarmingly high proportion of newly detected visible lesions and pathology grade change were found when patients were referred from the community to expert centers supporting the need for centralized care for BE-related neoplasia patients.
Disclosures:
Christian Davis, MD1, Andrew Fuller, MD2, David A. Katzka, MD3, Sachin Wani, MD1, Tarek Sawas, MD, MPH2. E0196 - The Impact of Centralized Care in the Management of Barrett’s Related Neoplasia: A Systematic Review and Meta-Analysis, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
Christian Davis, MD1, Andrew Fuller, MD2, David A. Katzka, MD3, Sachin Wani, MD1, Tarek Sawas, MD, MPH2
1University of Colorado, Anschutz Medical Center, Aurora, CO; 2University of Texas Southwestern, Dallas, TX; 3Columbia University, New York, NY
Introduction: Endoscopic eradication therapy (EET) is well-established for management of Barrett’s esophagus (BE) related neoplasia and increasingly being performed at tertiary care and community centers. While it has been suggested that these patients should be evaluated at expert centers, the impact of this practice has not been evaluated. We aimed to assess the impact of referral of BE-related neoplasia patients to expert centers by performing a systematic review and a meta-analysis and assessing the proportion of patients with change in pathologic diagnosis and visible lesions detected.
Methods: We searched multiple databases from inception until December 2021 for studies of patients with BE found in the community and referred to an expert center. Studies were included if they reported endoscopic and/or histologic findings in the community and after referral to an expert center. Studies were excluded if conducted in one setting only, insufficient data to determine the number of new visible lesions or pathology grade and studies with fewer than 10 subjects. The proportions of newly detected visible lesions and pathology grade change were pooled and weighted using a random effects model.
Results: Twelve studies met inclusion criteria that included 1829 patients. The pooled proportion of newly detected visible lesions was 45% (95% CI: 28%-63%, I2: 93.9%) (Figure A). The pooled proportion of pathology grade change when reviewed at an expert center was 45% (95% CI: 34%-56%, I2: 95.3%) (Figure B). The pooled proportion of pathology grade change after the endoscopy was repeated at an expert center was 47% (95%: 26% - 69%, I2: 97.2%). Patients referred with low-grade dysplasia (LGD) to expert centers had a pooled proportion of newly detectable visible lesions of 27% (95% CI: 22% - 32%, I2: 0%). The pooled proportion of pathologic grade change in patients referred with LGD when reviewed by an expert GI pathologist was 59% (95% CI: 40% - 77%, I2: 96.3%) and after repeat endoscopy was 40% (95% CI: 34% - 45%).
Discussion: An alarmingly high proportion of newly detected visible lesions and pathology grade change were found when patients were referred from the community to expert centers supporting the need for centralized care for BE-related neoplasia patients.
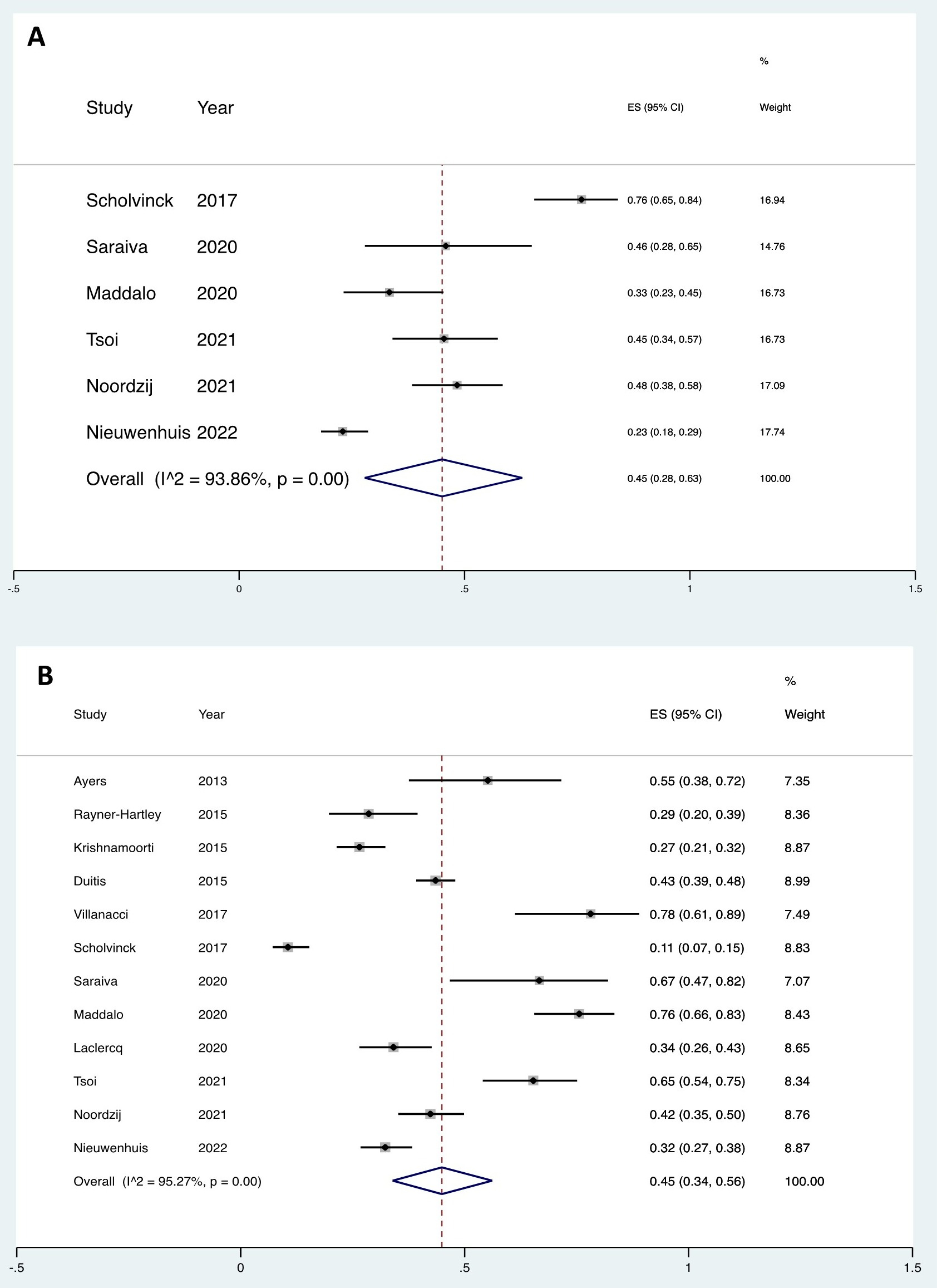
Figure: Figure: Forest plot of pooled proportions of newly detected visible lesions among patients with BE related neoplasia referred from the community to expert centers (A). Forest plot of pooled proportions of pathological grade change among patients with BE related neoplasia referred from the community to expert centers (B).
Disclosures:
Christian Davis indicated no relevant financial relationships.
Andrew Fuller indicated no relevant financial relationships.
David Katzka: celgene – Consultant. Takeda – Consultant.
Sachin Wani: Ambu – Grant/Research Support. CDx Medical – Grant/Research Support. Cernostics – Consultant. Exact Sciences – Consultant. Lucid Medical – Grant/Research Support.
Tarek Sawas indicated no relevant financial relationships.
Christian Davis, MD1, Andrew Fuller, MD2, David A. Katzka, MD3, Sachin Wani, MD1, Tarek Sawas, MD, MPH2. E0196 - The Impact of Centralized Care in the Management of Barrett’s Related Neoplasia: A Systematic Review and Meta-Analysis, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.

