Back
Poster Session B - Monday Morning
Category: Colon
B0118 - Colonic Mucormycosis as a Complication of COVID Pneumonia: A Case Report
Monday, October 24, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom
- KL
Kevin Lamm, MD
Prisma Health
Greenville, South Carolina
Presenting Author(s)
Award: Presidential Poster Award
Kevin Lamm, MD, Christina Bauer, MD, Samuel Horton, MD
Prisma Health, Greenville, SC
Introduction: Gastrointestinal mucormycosis is a rare infection with high mortality. Immunosuppression and uncontrolled diabetes are known to be significant risk factors for development of mucormycosis. The most common presenting symptoms include abdominal pain, fever, and perforation. Delay in diagnosis by 6 days has been shown to increase 30-day mortality from 35% to 66%. We present a case of colonic mucormycosis in a patient recovering from acute hypoxemic respiratory failure due to COVID-19 pneumonia.
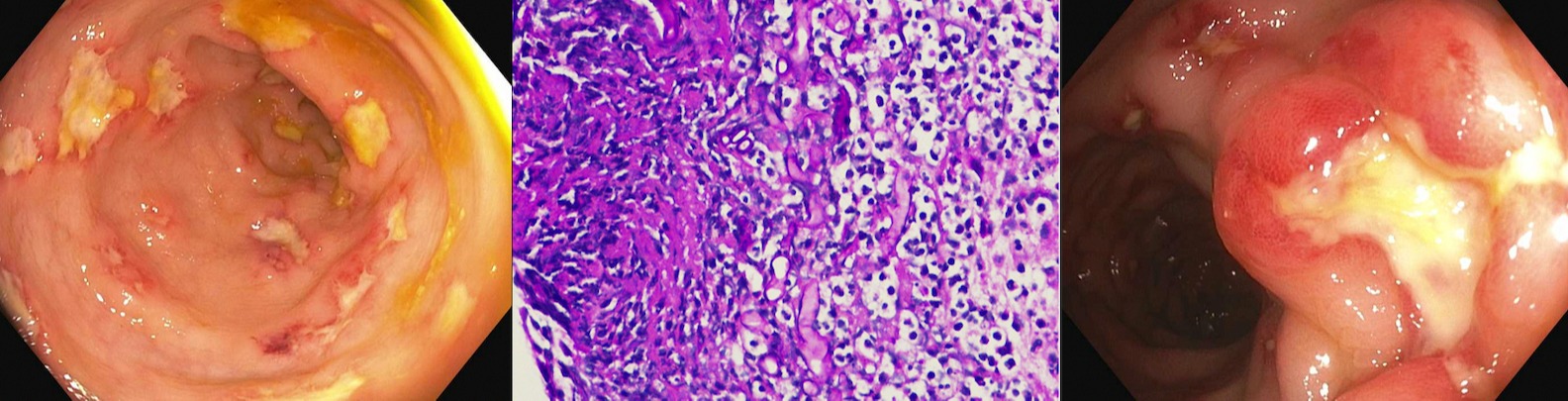
Case Description/Methods: A 31-year-old male with a remote history of appendiceal neuroendocrine tumor status post right hemicolectomy and uncontrolled type 1 diabetes presented with acute hypoxemic respiratory failure due to COVID-19 pneumonia. He was treated with dexamethasone. His course was complicated by sepsis due to polymicrobial bacteremia including culture growth of MSSA, E. faecalis and Enterobacter aerogenes. Gastroenterology was consulted for diarrhea, characterized as non-bloody, watery stools up to 10 times daily. Work-up was significant for negative fecal elastase, infectious studies including Giardia, negative celiac studies, HIV, TSH and autoimmune studies. Due to concern for enteropathy or microscopic colitis, upper and lower endoscopies were performed. Colonoscopy findings were significant for multiple punched-out ulcers in the rectum, rectosigmoid colon, and sigmoid colon. Sigmoid colon biopsies were significant for the presence of fungal organisms consistent with colonic mucormycosis. Given significant pathologic findings, ongoing fevers in the setting of broad-spectrum antibiotics, rising inflammatory markers, and positive serum beta-D-glucan assay patient was treated with IV Amphotericin for 2 months. His diarrhea improved and he has not had recurrence of disease, now 10 months later.
Discussion: The COVID-19 pandemic continues to bring unprecedented challenges to all facets of healthcare. We presented a rare case of colonic mucormycosis in the setting of uncontrolled Type I diabetes, COVID-19, and systemic corticosteroids. According to a systematic review of 70 adult case reports of gastrointestinal mucormycosis, 97% of patients were diagnosed with histopathologic examination whereas culture and molecular methods were used in only 28% and 17%, respectively. In our case, eradication of the invasive fungal infection and patient survival were attributable to prompt diagnosis.
Disclosures:
Kevin Lamm, MD, Christina Bauer, MD, Samuel Horton, MD. B0118 - Colonic Mucormycosis as a Complication of COVID Pneumonia: A Case Report, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
Kevin Lamm, MD, Christina Bauer, MD, Samuel Horton, MD
Prisma Health, Greenville, SC
Introduction: Gastrointestinal mucormycosis is a rare infection with high mortality. Immunosuppression and uncontrolled diabetes are known to be significant risk factors for development of mucormycosis. The most common presenting symptoms include abdominal pain, fever, and perforation. Delay in diagnosis by 6 days has been shown to increase 30-day mortality from 35% to 66%. We present a case of colonic mucormycosis in a patient recovering from acute hypoxemic respiratory failure due to COVID-19 pneumonia.
Case Description/Methods: A 31-year-old male with a remote history of appendiceal neuroendocrine tumor status post right hemicolectomy and uncontrolled type 1 diabetes presented with acute hypoxemic respiratory failure due to COVID-19 pneumonia. He was treated with dexamethasone. His course was complicated by sepsis due to polymicrobial bacteremia including culture growth of MSSA, E. faecalis and Enterobacter aerogenes. Gastroenterology was consulted for diarrhea, characterized as non-bloody, watery stools up to 10 times daily. Work-up was significant for negative fecal elastase, infectious studies including Giardia, negative celiac studies, HIV, TSH and autoimmune studies. Due to concern for enteropathy or microscopic colitis, upper and lower endoscopies were performed. Colonoscopy findings were significant for multiple punched-out ulcers in the rectum, rectosigmoid colon, and sigmoid colon. Sigmoid colon biopsies were significant for the presence of fungal organisms consistent with colonic mucormycosis. Given significant pathologic findings, ongoing fevers in the setting of broad-spectrum antibiotics, rising inflammatory markers, and positive serum beta-D-glucan assay patient was treated with IV Amphotericin for 2 months. His diarrhea improved and he has not had recurrence of disease, now 10 months later.
Discussion: The COVID-19 pandemic continues to bring unprecedented challenges to all facets of healthcare. We presented a rare case of colonic mucormycosis in the setting of uncontrolled Type I diabetes, COVID-19, and systemic corticosteroids. According to a systematic review of 70 adult case reports of gastrointestinal mucormycosis, 97% of patients were diagnosed with histopathologic examination whereas culture and molecular methods were used in only 28% and 17%, respectively. In our case, eradication of the invasive fungal infection and patient survival were attributable to prompt diagnosis.
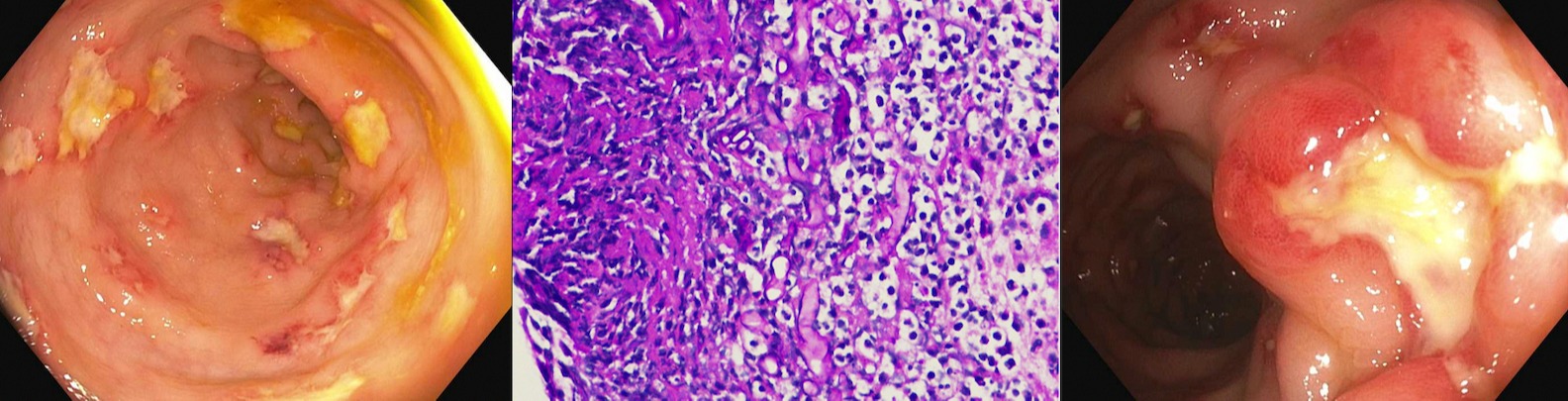
Figure: Left, Right: punched out, deep ulcerations of the sigmoid colon
Middle: PAS 400X. Fungal organisms present, consistent with mucormycosis in a background of acute inflammation, ulceration, and focal necrosis.
Middle: PAS 400X. Fungal organisms present, consistent with mucormycosis in a background of acute inflammation, ulceration, and focal necrosis.
Disclosures:
Kevin Lamm indicated no relevant financial relationships.
Christina Bauer indicated no relevant financial relationships.
Samuel Horton indicated no relevant financial relationships.
Kevin Lamm, MD, Christina Bauer, MD, Samuel Horton, MD. B0118 - Colonic Mucormycosis as a Complication of COVID Pneumonia: A Case Report, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.

