Back

Poster Session D - Tuesday Morning
Category: Stomach
D0720 - Cocaine and Non-Steroidal Anti-Inflammatory Drug-Induced Perforating Ulcer: The Case of the Double Lumen
Tuesday, October 25, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom
Has Audio
- KA
Kamal Amer, MD
Rutgers New Jersey Medical School
Newark, NJ
Presenting Author(s)
Kamal Amer, MD1, Brooke Baker, MS, MD2, Dayna Panchal, DO1, Maggie Cheung, MD1, Christopher Lenza, DO3
1Rutgers New Jersey Medical School, Newark, NJ; 2Rutgers-New Jersey Medical School, Newark, NJ; 3East Orange Veteran's Association, East Orange, NJ
Introduction: Peptic ulcers disease (PUD), or defects in the gastric or duodenal mucosa from a plethora of etiologies, account for over 750 million dollars in medical spending yearly. Although rare etiologies of PUD include infections, vascular insufficiency, infiltrating diseases as well as hormonal hyper secretion states, most common etiologies include Helicobacter pylori (H. Pylori) and Non-Steroidal Anti-inflammatory Drug (NSAID) use. Prior studies have demonstrated a synergistic effect of etiologies in forming PUD as well as increasing risks of complications, especially when discussing alternative medications and NSAID use. Here, we present an interesting endoscopic finding of a perforated peptic ulcer with fistualization into the duodenal bulb discovered during endoscopic evaluation for melena, likely secondary to vascular insufficiency and chronic NSAID use.
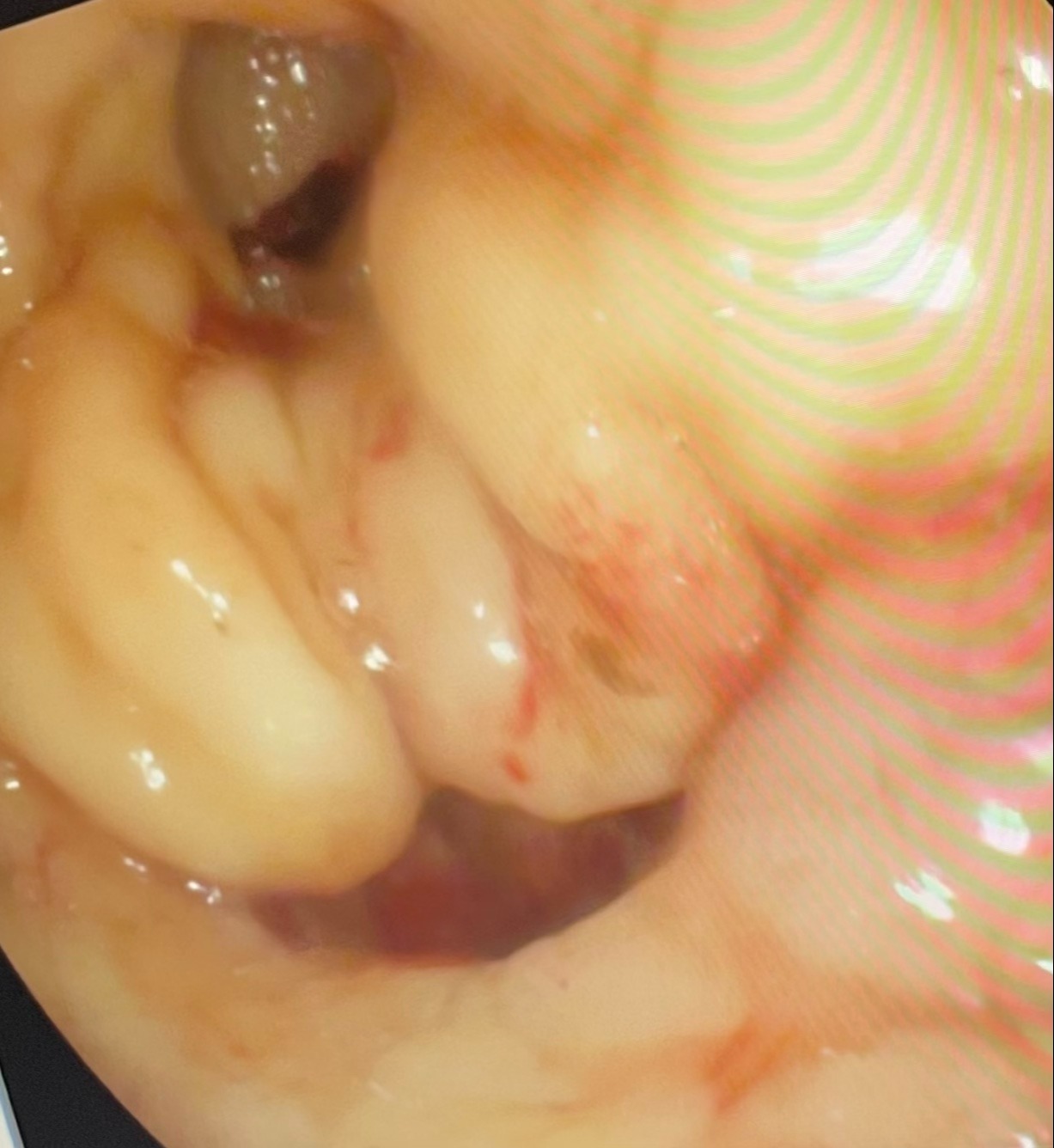
Case Description/Methods: This is a 73-year-old male with a medical history of hypertension, hyperlipidemia, ply-substance abuse (cocaine and marijuana), and peripheral artery disease who presented for evaluation of worsening pain and dry gangrene along his second to fourth toes. He underwent an emergent amputation as well as a left femoral to right femoral bypass with vascular surgery. He was loaded on clopidogrel and was admitted to medicine. Twelve hours after his procedure, he developed significant hypotension, tachycardia, and began to endorse melenic stools. An endoscopy showed frank blood in the stomach, duodenal bulb, and duodenum. After lavage of the blood, a lumen was visualized near the pylorus which was able to be traversed via the endoscopy scope. The lumen had areas of ulceration and bleeding, without any visible vessels. [Figure 1].
Discussion: The most common causes of PUD in the United States are NSAID use and H Pylori. This is further accentuated by vascular compromising agents such as cocaine. Cocaine is known to cause many gastrointestinal complications including bowel ischemia and gangrene. Most often gastric ulcers secondary to cocaine are found in the prepyloric/pyloric region and the first portion of the duodenum, consistent with this patient's presentation.
This patient had a gastroduodenal fistula, also known as an acquired double pylorus which was likely secondary to perforated ulcer in the prepyloric region. The double pylorus is a rare finding, and has been reported in 0.001% to 0.4% of upper gastrointestinal tract endoscopies. It is interesting that this patient endorsed no abdominal pain or dyspepsia.
Disclosures:
Kamal Amer, MD1, Brooke Baker, MS, MD2, Dayna Panchal, DO1, Maggie Cheung, MD1, Christopher Lenza, DO3. D0720 - Cocaine and Non-Steroidal Anti-Inflammatory Drug-Induced Perforating Ulcer: The Case of the Double Lumen, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1Rutgers New Jersey Medical School, Newark, NJ; 2Rutgers-New Jersey Medical School, Newark, NJ; 3East Orange Veteran's Association, East Orange, NJ
Introduction: Peptic ulcers disease (PUD), or defects in the gastric or duodenal mucosa from a plethora of etiologies, account for over 750 million dollars in medical spending yearly. Although rare etiologies of PUD include infections, vascular insufficiency, infiltrating diseases as well as hormonal hyper secretion states, most common etiologies include Helicobacter pylori (H. Pylori) and Non-Steroidal Anti-inflammatory Drug (NSAID) use. Prior studies have demonstrated a synergistic effect of etiologies in forming PUD as well as increasing risks of complications, especially when discussing alternative medications and NSAID use. Here, we present an interesting endoscopic finding of a perforated peptic ulcer with fistualization into the duodenal bulb discovered during endoscopic evaluation for melena, likely secondary to vascular insufficiency and chronic NSAID use.
Case Description/Methods: This is a 73-year-old male with a medical history of hypertension, hyperlipidemia, ply-substance abuse (cocaine and marijuana), and peripheral artery disease who presented for evaluation of worsening pain and dry gangrene along his second to fourth toes. He underwent an emergent amputation as well as a left femoral to right femoral bypass with vascular surgery. He was loaded on clopidogrel and was admitted to medicine. Twelve hours after his procedure, he developed significant hypotension, tachycardia, and began to endorse melenic stools. An endoscopy showed frank blood in the stomach, duodenal bulb, and duodenum. After lavage of the blood, a lumen was visualized near the pylorus which was able to be traversed via the endoscopy scope. The lumen had areas of ulceration and bleeding, without any visible vessels. [Figure 1].
Discussion: The most common causes of PUD in the United States are NSAID use and H Pylori. This is further accentuated by vascular compromising agents such as cocaine. Cocaine is known to cause many gastrointestinal complications including bowel ischemia and gangrene. Most often gastric ulcers secondary to cocaine are found in the prepyloric/pyloric region and the first portion of the duodenum, consistent with this patient's presentation.
This patient had a gastroduodenal fistula, also known as an acquired double pylorus which was likely secondary to perforated ulcer in the prepyloric region. The double pylorus is a rare finding, and has been reported in 0.001% to 0.4% of upper gastrointestinal tract endoscopies. It is interesting that this patient endorsed no abdominal pain or dyspepsia.
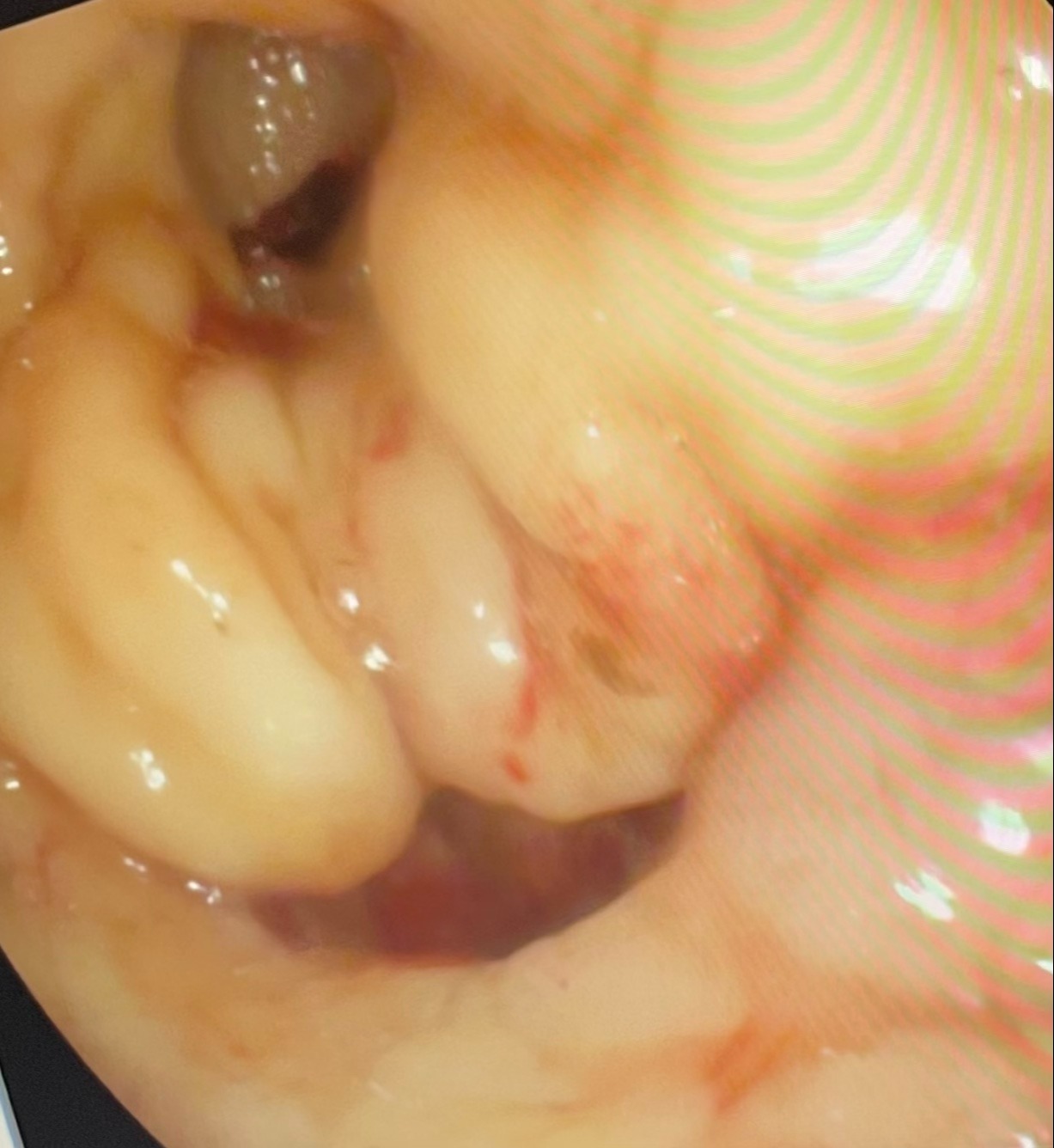
Figure: Endoscopic view of pylorus and pathologic lumen
Disclosures:
Kamal Amer indicated no relevant financial relationships.
Brooke Baker indicated no relevant financial relationships.
Dayna Panchal indicated no relevant financial relationships.
Maggie Cheung indicated no relevant financial relationships.
Christopher Lenza indicated no relevant financial relationships.
Kamal Amer, MD1, Brooke Baker, MS, MD2, Dayna Panchal, DO1, Maggie Cheung, MD1, Christopher Lenza, DO3. D0720 - Cocaine and Non-Steroidal Anti-Inflammatory Drug-Induced Perforating Ulcer: The Case of the Double Lumen, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
