Back

Poster Session B - Monday Morning
Category: Colon
B0121 - Pseudomyxoma peritonei - “Jelly Belly”: To Tap or Not?
Monday, October 24, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom
Has Audio

George Koutras, DO
Carepoint Health - Bayonne Medical Center
Bayonne, NJ
Presenting Author(s)
George Koutras, DO1, Neil Sondhi, MD1, Kovil Ramasamy, MD2, Devarajan Iyengar, MD1, John Dedousis, MD1, Antonios Tsompanidis, MD1
1Carepoint Health - Bayonne Medical Center, Bayonne, NJ; 2CarePoint Health - Bayonne Medical Center, Bayonne, NJ
Introduction: Mucinous adenocarcinomas of the appendix are defined as epithelial neoplasms often causing cystic dilation of the appendix due to accumulation of gelatinous material. Pseudomyxoma peritonei is an extremely rare complication of appendiceal mucinous adenocarcinomas with an estimated incidence rate of one to two people per million per year. Here-in we present a unique case of enterocutaneous fistula formation secondary to percutaneous biopsy of an enlarging omental mass in the setting of pseudomyxoma peritonei.
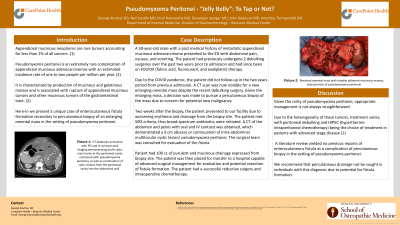
Case Description/Methods: A 50-year-old male with a past medical history of metastatic appendiceal mucinous adenocarcinoma presented to the ED with abdominal pain, nausea, and vomiting. The patient had previously undergone 2 debulking surgeries over the past two years prior to admission and has since been on FOLFOX therapy. Due to the COVID pandemic, the patient did not follow-up in the two years period from previous admission. A CT scan was now notable for a new enlarging omental mass despite the recent debulking surgery. Given the enlarging mass, a decision was made to pursue a percutaneous biopsy of the mass due to concern for potential new malignancy. Two weeks after the biopsy, the patient presented to our facility due to worsening erythema and drainage from the biopsy site. The patient met SIRS criteria, thus broad-spectrum antibiotics were initiated. A CT of the abdomen and pelvis with oral and IV contrast was obtained, which demonstrated a 9 cm abscess or continuation of intra-abdominal multilocular cystic lesion/ pseudomyxoma peritonei. The surgical team was consulted. Patient had 100 cc of purulent and mucinous drainage expressed from biopsy site. The patient was then placed for transfer to a hospital capable of advanced surgical management for evaluation and potential resection of fistula formation. The patient had a successful reductive surgery and intraoperative chemotherapy.
Discussion: Given the rarity of pseudomyxoma peritonei, appropriate management is not always straightforward. A literature review yielded no previous reports of enterocutaneous fistula as a complication of percutaneous drainage in the setting of pseudomyxoma peritonei. We recommend that percutaneous drainage not be sought in individuals with this diagnosis due to potential for fistula formation.

Disclosures:
George Koutras, DO1, Neil Sondhi, MD1, Kovil Ramasamy, MD2, Devarajan Iyengar, MD1, John Dedousis, MD1, Antonios Tsompanidis, MD1. B0121 - Pseudomyxoma peritonei - “Jelly Belly”: To Tap or Not?, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1Carepoint Health - Bayonne Medical Center, Bayonne, NJ; 2CarePoint Health - Bayonne Medical Center, Bayonne, NJ
Introduction: Mucinous adenocarcinomas of the appendix are defined as epithelial neoplasms often causing cystic dilation of the appendix due to accumulation of gelatinous material. Pseudomyxoma peritonei is an extremely rare complication of appendiceal mucinous adenocarcinomas with an estimated incidence rate of one to two people per million per year. Here-in we present a unique case of enterocutaneous fistula formation secondary to percutaneous biopsy of an enlarging omental mass in the setting of pseudomyxoma peritonei.
Case Description/Methods: A 50-year-old male with a past medical history of metastatic appendiceal mucinous adenocarcinoma presented to the ED with abdominal pain, nausea, and vomiting. The patient had previously undergone 2 debulking surgeries over the past two years prior to admission and has since been on FOLFOX therapy. Due to the COVID pandemic, the patient did not follow-up in the two years period from previous admission. A CT scan was now notable for a new enlarging omental mass despite the recent debulking surgery. Given the enlarging mass, a decision was made to pursue a percutaneous biopsy of the mass due to concern for potential new malignancy. Two weeks after the biopsy, the patient presented to our facility due to worsening erythema and drainage from the biopsy site. The patient met SIRS criteria, thus broad-spectrum antibiotics were initiated. A CT of the abdomen and pelvis with oral and IV contrast was obtained, which demonstrated a 9 cm abscess or continuation of intra-abdominal multilocular cystic lesion/ pseudomyxoma peritonei. The surgical team was consulted. Patient had 100 cc of purulent and mucinous drainage expressed from biopsy site. The patient was then placed for transfer to a hospital capable of advanced surgical management for evaluation and potential resection of fistula formation. The patient had a successful reductive surgery and intraoperative chemotherapy.
Discussion: Given the rarity of pseudomyxoma peritonei, appropriate management is not always straightforward. A literature review yielded no previous reports of enterocutaneous fistula as a complication of percutaneous drainage in the setting of pseudomyxoma peritonei. We recommend that percutaneous drainage not be sought in individuals with this diagnosis due to potential for fistula formation.

Figure: Above is the resected omental mass that led to fistula formation post percutaneous biopsy. Cytogenetics yielded that this tumor was of a different genotype than the patient's original cancer.
Disclosures:
George Koutras indicated no relevant financial relationships.
Neil Sondhi indicated no relevant financial relationships.
Kovil Ramasamy indicated no relevant financial relationships.
Devarajan Iyengar indicated no relevant financial relationships.
John Dedousis indicated no relevant financial relationships.
Antonios Tsompanidis indicated no relevant financial relationships.
George Koutras, DO1, Neil Sondhi, MD1, Kovil Ramasamy, MD2, Devarajan Iyengar, MD1, John Dedousis, MD1, Antonios Tsompanidis, MD1. B0121 - Pseudomyxoma peritonei - “Jelly Belly”: To Tap or Not?, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
