Back


Poster Session E - Tuesday Afternoon
Category: GI Bleeding
E0328 - It Is so Complicated: Pancreatico-Spleno-Colonic Fistula Presenting as Gastrointestinal Bleeding
Tuesday, October 25, 2022
3:00 PM – 5:00 PM ET
Location: Crown Ballroom

Has Audio
- OS
Oluwaseun Shogbesan, MPH, MD
Tower Health - Reading Hospital
Sinking Spring, PA
Presenting Author(s)
Oluwaseun Shogbesan, MPH, MD1, Dhruv Patel, MD2, John Altomare, MD3, Gbenga Shogbesan, MD2
1Tower Health - Reading Hospital, Sinking Spring, PA; 2Emory University Hospital, Atlanta, GA; 3Tower Health - Reading Hospital, Reading, PA
Introduction: Gastrointestinal bleeding is common in clinical practice with variable etiology, we present a rare case of pancreatic pseudocyst complicated by spleno-colonic fistula manifesting with brisk hematochezia.
Case Description/Methods: A 50-year-old male with no significant past medical history presented with fever and acute encephalopathy. He subsequently had a prolonged and complicated hospital course with a new diagnosis of Human immunodeficiency virus/Acquired immunodeficiency
syndrome, disseminated tuberculosis, and chronic pancreatitis with a pancreatic pseudocyst.
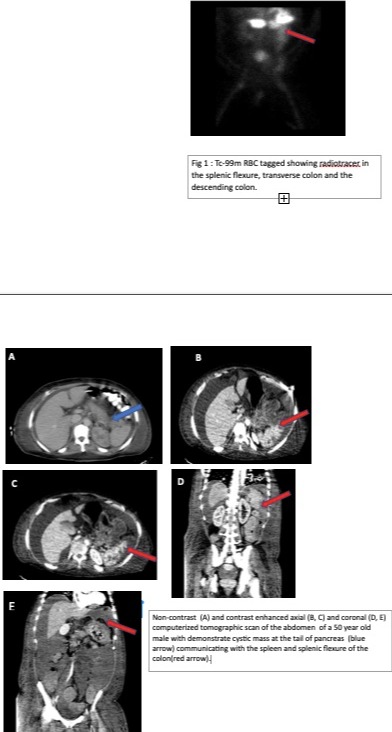
During hospitalization, the patient suddenly developed passage of bright red blood per rectum over 48 hours with down-trending hemoglobin. Hemoglobin initially dropped from 9.6 g/dL to 5.0 g/dl (Normal: 12-16g/dL) and he required multiple units of packed red cell, platelets, and fresh frozen plasma transfusion. The patient underwent a tagged Red blood cell scan with radiolabelled 28.4 mCi of Tc-99m. Red blood cell tagged Tc 99m gastrointestinal bleeding scan showed large brisk pooling of the radiotracer in the splenic flexure consistent with significant active hemorrhage in the region of the splenic flexure. There was a retrograde flow of the tracer into the transverse colon and antegrade flow into the descending colon. Retrospective evaluation of the prior CT tomography scans of the abdomen demonstrated possible communication between the pancreatic tail cyst, the spleen as well as the splenic flexure which was the likely source of the GI bleed. The patient had a total of 35 units of packed red blood cells transfused, 8 units of platelets, and 7 units of fresh frozen plasma during his hospital course. The patient failed multiple attempts at Interventional radiology arterial embolization and due to multiple co-morbidities, he was not a candidate for surgical intervention. He later died after 6 months of hospitalization.
Discussion: There have been reported cases of pancreatico-colonic fistula and spleno-colonic fistula, arising from pancreatic pseudocysts and pseudoaneurysms associated with trauma, pancreatitis, and Crohn’s disease. Pancreatico-spleno-colonic fistula is a rare and complex entity usually presenting with massive gastrointestinal bleeding. The findings of acute or chronic pancreatitis and pseudocyst with gastrointestinal bleeding should raise the suspicion of possible pancreatico-colonic fistula. Prompt imaging is key to accurate diagnosis and management.
Disclosures:
Oluwaseun Shogbesan, MPH, MD1, Dhruv Patel, MD2, John Altomare, MD3, Gbenga Shogbesan, MD2. E0328 - It Is so Complicated: Pancreatico-Spleno-Colonic Fistula Presenting as Gastrointestinal Bleeding, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1Tower Health - Reading Hospital, Sinking Spring, PA; 2Emory University Hospital, Atlanta, GA; 3Tower Health - Reading Hospital, Reading, PA
Introduction: Gastrointestinal bleeding is common in clinical practice with variable etiology, we present a rare case of pancreatic pseudocyst complicated by spleno-colonic fistula manifesting with brisk hematochezia.
Case Description/Methods: A 50-year-old male with no significant past medical history presented with fever and acute encephalopathy. He subsequently had a prolonged and complicated hospital course with a new diagnosis of Human immunodeficiency virus/Acquired immunodeficiency
syndrome, disseminated tuberculosis, and chronic pancreatitis with a pancreatic pseudocyst.
During hospitalization, the patient suddenly developed passage of bright red blood per rectum over 48 hours with down-trending hemoglobin. Hemoglobin initially dropped from 9.6 g/dL to 5.0 g/dl (Normal: 12-16g/dL) and he required multiple units of packed red cell, platelets, and fresh frozen plasma transfusion. The patient underwent a tagged Red blood cell scan with radiolabelled 28.4 mCi of Tc-99m. Red blood cell tagged Tc 99m gastrointestinal bleeding scan showed large brisk pooling of the radiotracer in the splenic flexure consistent with significant active hemorrhage in the region of the splenic flexure. There was a retrograde flow of the tracer into the transverse colon and antegrade flow into the descending colon. Retrospective evaluation of the prior CT tomography scans of the abdomen demonstrated possible communication between the pancreatic tail cyst, the spleen as well as the splenic flexure which was the likely source of the GI bleed. The patient had a total of 35 units of packed red blood cells transfused, 8 units of platelets, and 7 units of fresh frozen plasma during his hospital course. The patient failed multiple attempts at Interventional radiology arterial embolization and due to multiple co-morbidities, he was not a candidate for surgical intervention. He later died after 6 months of hospitalization.
Discussion: There have been reported cases of pancreatico-colonic fistula and spleno-colonic fistula, arising from pancreatic pseudocysts and pseudoaneurysms associated with trauma, pancreatitis, and Crohn’s disease. Pancreatico-spleno-colonic fistula is a rare and complex entity usually presenting with massive gastrointestinal bleeding. The findings of acute or chronic pancreatitis and pseudocyst with gastrointestinal bleeding should raise the suspicion of possible pancreatico-colonic fistula. Prompt imaging is key to accurate diagnosis and management.
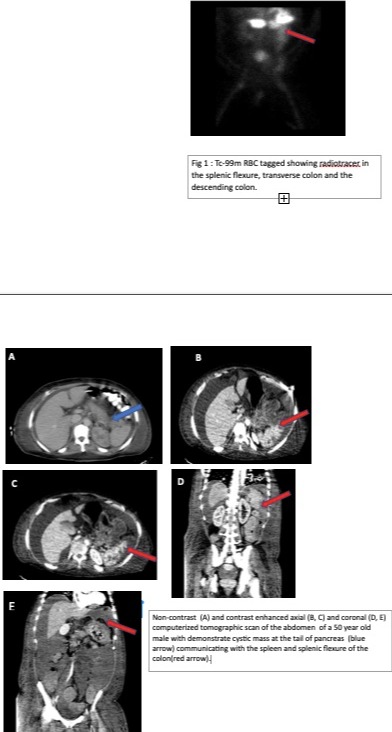
Figure: Fig 1: Tc-99m RBC tagged showing radiotracer in the splenic flexure, transverse colon and the descending colon.
Non-contrast (A) and contrast enhanced axial (B, C) and coronal (D, E) computerized tomographic scan of the abdomen showing cystic mass at the tail of pancreas (blue arrow) communicating with the spleen and splenic flexure of the colon(red arrow).
Non-contrast (A) and contrast enhanced axial (B, C) and coronal (D, E) computerized tomographic scan of the abdomen showing cystic mass at the tail of pancreas (blue arrow) communicating with the spleen and splenic flexure of the colon(red arrow).
Disclosures:
Oluwaseun Shogbesan indicated no relevant financial relationships.
Dhruv Patel indicated no relevant financial relationships.
John Altomare indicated no relevant financial relationships.
Gbenga Shogbesan indicated no relevant financial relationships.
Oluwaseun Shogbesan, MPH, MD1, Dhruv Patel, MD2, John Altomare, MD3, Gbenga Shogbesan, MD2. E0328 - It Is so Complicated: Pancreatico-Spleno-Colonic Fistula Presenting as Gastrointestinal Bleeding, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
