Back

Poster Session D - Tuesday Morning
Category: Colon
D0147 - A Case of GI Tract Involvement in a Patient Presenting With Granulomatosis With Polyangiitis
Tuesday, October 25, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom
Has Audio

Samuel Tanner, MD
University Hospitals Cleveland Medical Center
Cleveland, OH
Presenting Author(s)
Samuel Tanner, MD, Ahmad Khan, MD, Amitabh Chak, MD
University Hospitals Cleveland Medical Center, Cleveland, OH
Introduction: The differential for colitis is broad, including infectious, ischemic, diverticulitis, inflammatory bowel disease and vasculitis etiologies. In this report, we present the case of a patient who presented with acute anemia in the setting of colitis along with chronic sinusitis, palpable purpura, and acute renal failure who was eventually found to have granulomatosis with polyangiitis (GPA).
Case Description/Methods: A 51-year-old man with a three-month history of sinusitis refractory to antibiotics presented with a two-week history of diarrhea with intermittent melanic stools and a nonpainful, nonpruritic palpable purpuric rash on his legs, feet (including soles) and palms. He was hemodynamically stable and abdominal exam was benign. His laboratory workup was significant for a leukocytosis of 18.2 (he had previously been started on steroids), hemoglobin 8.4g/dL (baseline 15g/dL), and creatinine of 1.8mg/dL from baseline 1.0mg/dL. He had no personal or family history of inflammatory bowel disease, other autoimmune disorders, or malignancy.
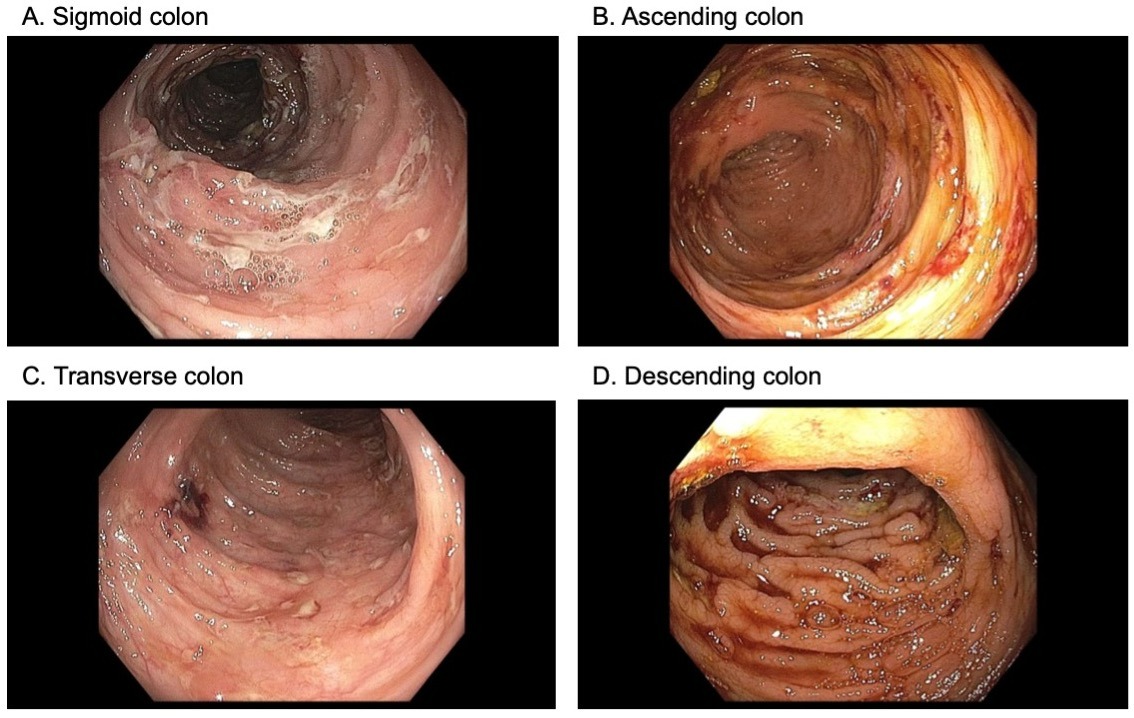
Colonoscopy revealed moderate to severe diffuse friable, ulcerated mucosa with punched out ulcers in the sigmoid, descending, transverse, and ascending colon (Figure). Biopsies revealed ulcerated mucosa without features of inflammatory bowel disease. Subsequent skin biopsy revealed leukocytoclastic vasculitis. Given his constellation of symptoms, he was presumed to have Henoch-Schonlein purpura. However, renal function declined and renal biopsy was pursued, which showed pauci-immune necrotizing crescentic glomerulonephritis. Subsequent workup showed positive c-ANCA / PR3, consistent with granulomatosis with polyangiitis. He was switched from PO to IV high dose steroids and initiated on rituximab and plasmapheresis with clinical resolution of symptoms.
Discussion: Classically, GPA is thought to be a disease affecting the lungs, skin, and kidney. GI tract involvement in GPA is rare, accounting for less than 10% of all cases. The diagnosis of GPA can be difficult as many initial symptoms can mimic other vasculitides or inflammatory bowel disease in the setting of GI tract involvement. However, prompt recognition of this disease is critical as early renal biopsy can confirm the diagnosis. In our patient, the combination of positive c-ANCA / PR3 with renal failure in the setting pauci-immune glomerulonephritis allowed to identify GPA and start therapy.
Disclosures:
Samuel Tanner, MD, Ahmad Khan, MD, Amitabh Chak, MD. D0147 - A Case of GI Tract Involvement in a Patient Presenting With Granulomatosis With Polyangiitis, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
University Hospitals Cleveland Medical Center, Cleveland, OH
Introduction: The differential for colitis is broad, including infectious, ischemic, diverticulitis, inflammatory bowel disease and vasculitis etiologies. In this report, we present the case of a patient who presented with acute anemia in the setting of colitis along with chronic sinusitis, palpable purpura, and acute renal failure who was eventually found to have granulomatosis with polyangiitis (GPA).
Case Description/Methods: A 51-year-old man with a three-month history of sinusitis refractory to antibiotics presented with a two-week history of diarrhea with intermittent melanic stools and a nonpainful, nonpruritic palpable purpuric rash on his legs, feet (including soles) and palms. He was hemodynamically stable and abdominal exam was benign. His laboratory workup was significant for a leukocytosis of 18.2 (he had previously been started on steroids), hemoglobin 8.4g/dL (baseline 15g/dL), and creatinine of 1.8mg/dL from baseline 1.0mg/dL. He had no personal or family history of inflammatory bowel disease, other autoimmune disorders, or malignancy.
Colonoscopy revealed moderate to severe diffuse friable, ulcerated mucosa with punched out ulcers in the sigmoid, descending, transverse, and ascending colon (Figure). Biopsies revealed ulcerated mucosa without features of inflammatory bowel disease. Subsequent skin biopsy revealed leukocytoclastic vasculitis. Given his constellation of symptoms, he was presumed to have Henoch-Schonlein purpura. However, renal function declined and renal biopsy was pursued, which showed pauci-immune necrotizing crescentic glomerulonephritis. Subsequent workup showed positive c-ANCA / PR3, consistent with granulomatosis with polyangiitis. He was switched from PO to IV high dose steroids and initiated on rituximab and plasmapheresis with clinical resolution of symptoms.
Discussion: Classically, GPA is thought to be a disease affecting the lungs, skin, and kidney. GI tract involvement in GPA is rare, accounting for less than 10% of all cases. The diagnosis of GPA can be difficult as many initial symptoms can mimic other vasculitides or inflammatory bowel disease in the setting of GI tract involvement. However, prompt recognition of this disease is critical as early renal biopsy can confirm the diagnosis. In our patient, the combination of positive c-ANCA / PR3 with renal failure in the setting pauci-immune glomerulonephritis allowed to identify GPA and start therapy.
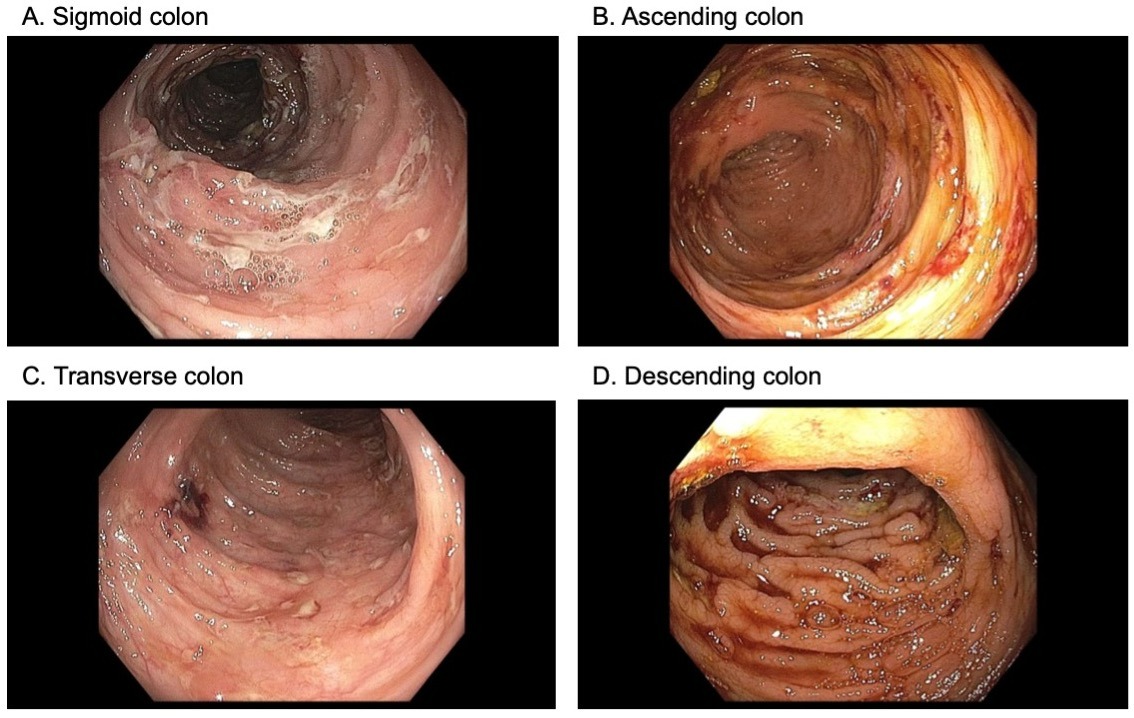
Figure: Figure. Colonoscopy showing moderate to severe diffuse friable, ulcerated mucosa with some bleeding. Punched out ulcers were noted in the sigmoid, descending, transverse, and ascending colon, as well as in the cecum with distal sigmoid and rectal sparing.
Disclosures:
Samuel Tanner indicated no relevant financial relationships.
Ahmad Khan indicated no relevant financial relationships.
Amitabh Chak: Lucid Diagnostics – Owner/Ownership Interest. Microtek – Consultant. US Endoscopy – Consultant.
Amitabh Chak — NO DISCLOSURE DATA.
Samuel Tanner, MD, Ahmad Khan, MD, Amitabh Chak, MD. D0147 - A Case of GI Tract Involvement in a Patient Presenting With Granulomatosis With Polyangiitis, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
