Back

Poster Session E - Tuesday Afternoon
Category: Liver
E0523 - Warfarin-Induced Skin Necrosis Following Routine Endoscopy in a Patient With Cirrhosis
Tuesday, October 25, 2022
3:00 PM – 5:00 PM ET
Location: Crown Ballroom
Has Audio

Franklyn Wallace, MD
Mayo Clinic Rochester
Rochester, MN
Presenting Author(s)
Franklyn Wallace, MD, Jennifer Kleinman Sween, MD
Mayo Clinic Rochester, Rochester, MN
Introduction: Warfarin-induced skin necrosis (WISN) is rare, and most cases are caused by inherited deficiencies of protein C. Acquired protein C deficiency has been associated with advanced liver disease, ulcerative colitis (UC), and malignancies. Due to its rarity, clinicians must have a high index of suspicion for WISN to avoid delays in diagnosis or treatment.
Case Description/Methods: A 67-year-old male with UC, cirrhosis due to primary biliary cholangitis, and prior pulmonary embolism on warfarin underwent surveillance EGD and colonoscopy. Warfarin was held for five days prior to the procedures without bridging. EGD was unremarkable and colonoscopy revealed active UC. He resumed warfarin therapy the next day.
Two days later, he developed significant tenderness and bruising on his abdomen, flank, and outer thighs. After evaluation by multiple providers, his pain was attributed to central sensitization, and he was prescribed gabapentin.
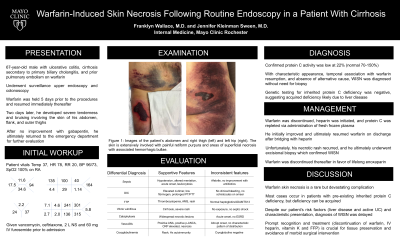
Over the next several days, he developed extensive painful retiform purpura and expanding areas of superficial necrosis (Figure 1). He was admitted to the hospital for multidisciplinary evaluation. Extensive workup assessed potential causes, such as WISN, sepsis, vasculitis, disseminated intravascular coagulation (DIC), thrombotic thrombocytopenic purpura (TTP), or cryoglobulinemia. Given the characteristic appearance and temporal association with restarting warfarin, WISN was thought to be the most likely etiology. Protein C activity was low at 22% (normal 70-150%). Genetic testing for inherited protein C deficiency was negative, confirming an acquired deficiency.
For management of WISN, warfarin was discontinued, heparin was initiated, and protein C was repleted with fresh frozen plasma (FFP). He was discharged on warfarin after bridging with heparin. He later had recurrence of his necrotic rash, and an excisional biopsy confirmed WISN. Warfarin was then discontinued in favor of lifelong enoxaparin.
Discussion: Our case highlights a rare but devastating complication of warfarin use. In WISN, protein C is depleted prior to other vitamin K-dependent factors, leading to a transient hypercoagulable state, microvascular occlusion, and tissue necrosis. Despite our patient’s risk factors (liver disease and active UC) and characteristic presentation, diagnosis of WISN was delayed. Prompt recognition and treatment (discontinuation of warfarin, IV heparin, vitamin K and FFP) is crucial for tissue preservation and avoidance of morbid surgical interventions.

Disclosures:
Franklyn Wallace, MD, Jennifer Kleinman Sween, MD. E0523 - Warfarin-Induced Skin Necrosis Following Routine Endoscopy in a Patient With Cirrhosis, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
Mayo Clinic Rochester, Rochester, MN
Introduction: Warfarin-induced skin necrosis (WISN) is rare, and most cases are caused by inherited deficiencies of protein C. Acquired protein C deficiency has been associated with advanced liver disease, ulcerative colitis (UC), and malignancies. Due to its rarity, clinicians must have a high index of suspicion for WISN to avoid delays in diagnosis or treatment.
Case Description/Methods: A 67-year-old male with UC, cirrhosis due to primary biliary cholangitis, and prior pulmonary embolism on warfarin underwent surveillance EGD and colonoscopy. Warfarin was held for five days prior to the procedures without bridging. EGD was unremarkable and colonoscopy revealed active UC. He resumed warfarin therapy the next day.
Two days later, he developed significant tenderness and bruising on his abdomen, flank, and outer thighs. After evaluation by multiple providers, his pain was attributed to central sensitization, and he was prescribed gabapentin.
Over the next several days, he developed extensive painful retiform purpura and expanding areas of superficial necrosis (Figure 1). He was admitted to the hospital for multidisciplinary evaluation. Extensive workup assessed potential causes, such as WISN, sepsis, vasculitis, disseminated intravascular coagulation (DIC), thrombotic thrombocytopenic purpura (TTP), or cryoglobulinemia. Given the characteristic appearance and temporal association with restarting warfarin, WISN was thought to be the most likely etiology. Protein C activity was low at 22% (normal 70-150%). Genetic testing for inherited protein C deficiency was negative, confirming an acquired deficiency.
For management of WISN, warfarin was discontinued, heparin was initiated, and protein C was repleted with fresh frozen plasma (FFP). He was discharged on warfarin after bridging with heparin. He later had recurrence of his necrotic rash, and an excisional biopsy confirmed WISN. Warfarin was then discontinued in favor of lifelong enoxaparin.
Discussion: Our case highlights a rare but devastating complication of warfarin use. In WISN, protein C is depleted prior to other vitamin K-dependent factors, leading to a transient hypercoagulable state, microvascular occlusion, and tissue necrosis. Despite our patient’s risk factors (liver disease and active UC) and characteristic presentation, diagnosis of WISN was delayed. Prompt recognition and treatment (discontinuation of warfarin, IV heparin, vitamin K and FFP) is crucial for tissue preservation and avoidance of morbid surgical interventions.

Figure: Figure 1: Images of the patient’s abdomen and right thigh (left) and left hip (right). The skin is extensively involved with painful retiform purpura and areas of superficial necrosis with associated hemorrhagic bullae.
Disclosures:
Franklyn Wallace indicated no relevant financial relationships.
Jennifer Kleinman Sween indicated no relevant financial relationships.
Franklyn Wallace, MD, Jennifer Kleinman Sween, MD. E0523 - Warfarin-Induced Skin Necrosis Following Routine Endoscopy in a Patient With Cirrhosis, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
