Back

Poster Session E - Tuesday Afternoon
Category: Liver
E0559 - The (Icteric) Eye of the Storm: A Case of Weil’s Syndrome
Tuesday, October 25, 2022
3:00 PM – 5:00 PM ET
Location: Crown Ballroom
Has Audio
.jpg)
Baruh B. Mulat
Montefiore Medical Center
Bronx, NY
Presenting Author(s)
Baruh B. Mulat, , Hilary Hertan, MD, FACG
Montefiore Medical Center, Bronx, NY
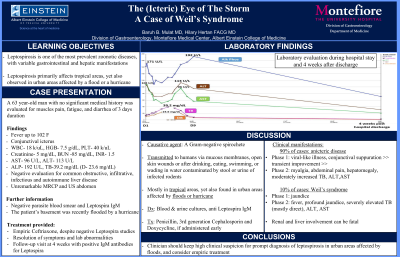
Introduction: Leptospirosis is one of the most prevalent zoonotic diseases affecting humans residing in tropical areas. We herein describe a case of a patient with leptospirosis acquired in the Bronx, NY.
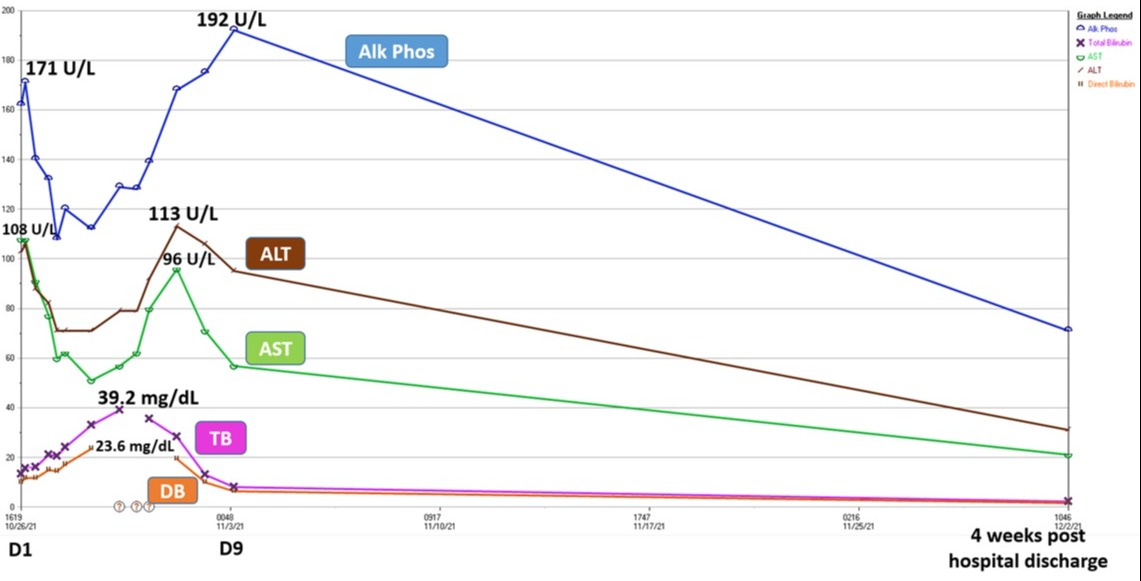
Case Description/Methods: A 63 year-old man with no significant medical history was evaluated for muscle pain, fatigue, and diarrhea of 3 days duration. He was feverish to 102 F and icteric. Laboratory evaluation revealed hemoglobin of 7.5 g/dL, total white count of 18 k/uL, platelet count of 40 k/uL, INR 1.5, creatinine of 5 mg/dL, urea nitrogen 85 mg/dL, creatine kinase 4000 U/L, alkaline phosphatase 192 U/L, total bilirubin 39 mg/dL, direct bilirubin > 23 mg/dL, AST 96 U/L, ALT 113 U/L and albumin 2.5 g/dL. Initial laboratory evaluation was negative for common and atypical infections. Radiologic evaluation revealed unremarkable non-contrast MRCP and US abdomen. Upon further detailed history, the patient reported that his basement was recently flooded by a devastating hurricane. Despite negative parasite blood smear and IgM antibodies for leptospira, empiric treatment for leptospirosis with Ceftriaxone resulted in resolution of all symptoms and lab abnormalities. Repeated blood work on follow-up visits at 4 weeks was noted with positive IgM antibodies for leptospira.
Discussion: Leptospirosis is caused by a poorly staining gram-negative spirochetal bacteria. Transmission to humans occurs through mucous membranes, open skin wounds or after drinking, eating, swimming, or wading in water contaminated by stool or urine of infected rodents. Outbreaks have been documented in non tropical, urban areas affected by hurricanes, heavy rains or floods. In approximately 90% of cases, the disease is anicteric. Phase 1 includes viral-like illness, conjunctival suppuration followed by transient improvement. Phase 2 includes myalgia, nausea, vomiting, abdominal pain, hepatomegaly, increased serum bilirubin and serum aminotransferases. 10% of cases manifest as Weil’s syndrome, characterized by jaundice in the first phase, followed by second phase manifesting with high fever, profound jaundice with severely elevated serum bilirubin levels (up to 30mg/dL, mostly direct) and elevated serum transaminases. Renal and liver involvement are predominant and can lead to severe morbidity and death. Blood cultures, urine cultures and specific anti Leptospira IgM serology can assist with diagnosis. Antibiotic treatments, primarily Penicillin, 3rd generation Cephalosporins and Doxycycline, can benefit if administered at an early stage.
Disclosures:
Baruh B. Mulat, , Hilary Hertan, MD, FACG. E0559 - The (Icteric) Eye of the Storm: A Case of Weil’s Syndrome, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
Montefiore Medical Center, Bronx, NY
Introduction: Leptospirosis is one of the most prevalent zoonotic diseases affecting humans residing in tropical areas. We herein describe a case of a patient with leptospirosis acquired in the Bronx, NY.
Case Description/Methods: A 63 year-old man with no significant medical history was evaluated for muscle pain, fatigue, and diarrhea of 3 days duration. He was feverish to 102 F and icteric. Laboratory evaluation revealed hemoglobin of 7.5 g/dL, total white count of 18 k/uL, platelet count of 40 k/uL, INR 1.5, creatinine of 5 mg/dL, urea nitrogen 85 mg/dL, creatine kinase 4000 U/L, alkaline phosphatase 192 U/L, total bilirubin 39 mg/dL, direct bilirubin > 23 mg/dL, AST 96 U/L, ALT 113 U/L and albumin 2.5 g/dL. Initial laboratory evaluation was negative for common and atypical infections. Radiologic evaluation revealed unremarkable non-contrast MRCP and US abdomen. Upon further detailed history, the patient reported that his basement was recently flooded by a devastating hurricane. Despite negative parasite blood smear and IgM antibodies for leptospira, empiric treatment for leptospirosis with Ceftriaxone resulted in resolution of all symptoms and lab abnormalities. Repeated blood work on follow-up visits at 4 weeks was noted with positive IgM antibodies for leptospira.
Discussion: Leptospirosis is caused by a poorly staining gram-negative spirochetal bacteria. Transmission to humans occurs through mucous membranes, open skin wounds or after drinking, eating, swimming, or wading in water contaminated by stool or urine of infected rodents. Outbreaks have been documented in non tropical, urban areas affected by hurricanes, heavy rains or floods. In approximately 90% of cases, the disease is anicteric. Phase 1 includes viral-like illness, conjunctival suppuration followed by transient improvement. Phase 2 includes myalgia, nausea, vomiting, abdominal pain, hepatomegaly, increased serum bilirubin and serum aminotransferases. 10% of cases manifest as Weil’s syndrome, characterized by jaundice in the first phase, followed by second phase manifesting with high fever, profound jaundice with severely elevated serum bilirubin levels (up to 30mg/dL, mostly direct) and elevated serum transaminases. Renal and liver involvement are predominant and can lead to severe morbidity and death. Blood cultures, urine cultures and specific anti Leptospira IgM serology can assist with diagnosis. Antibiotic treatments, primarily Penicillin, 3rd generation Cephalosporins and Doxycycline, can benefit if administered at an early stage.
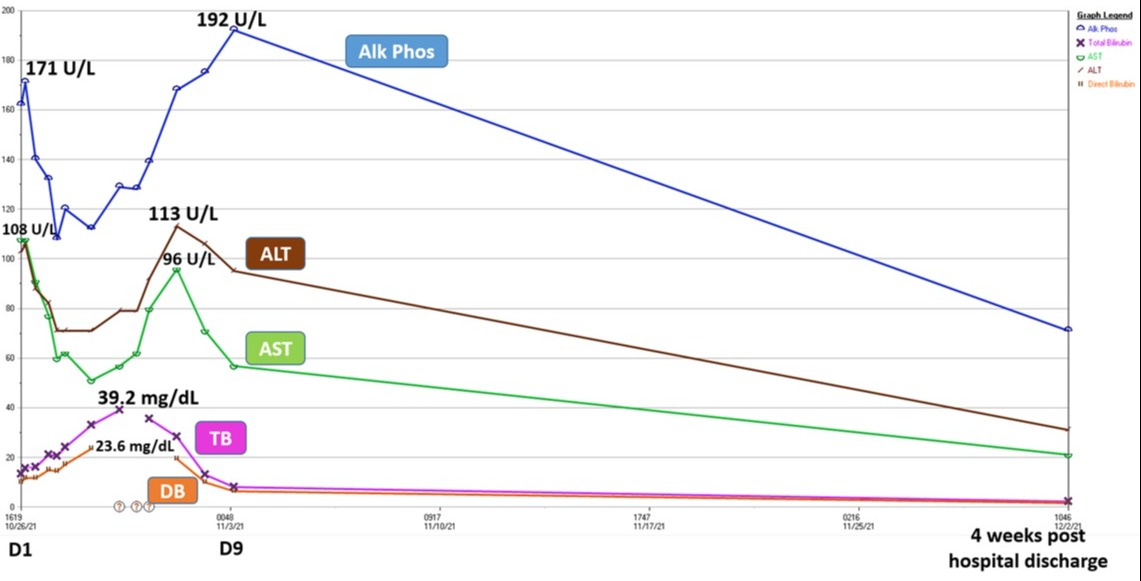
Figure: Figure 1- Laboratory evaluation during hospital stay and 4 weeks after discharge.
Abbreviation: ALP, alkaline phosphatase; TB, total bilirubin; DB, direct bilirubin; AST, Aspartate transaminase; ALT, Alanine transaminase;
Abbreviation: ALP, alkaline phosphatase; TB, total bilirubin; DB, direct bilirubin; AST, Aspartate transaminase; ALT, Alanine transaminase;
Disclosures:
Baruh Mulat indicated no relevant financial relationships.
Hilary Hertan indicated no relevant financial relationships.
Baruh B. Mulat, , Hilary Hertan, MD, FACG. E0559 - The (Icteric) Eye of the Storm: A Case of Weil’s Syndrome, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
