Back

Poster Session E - Tuesday Afternoon
Category: Liver
E0589 - A Budding Dilemma: A Rare Case of Sickle Cell Disease Causing Incidental Budd-Chiari Syndrome
Tuesday, October 25, 2022
3:00 PM – 5:00 PM ET
Location: Crown Ballroom
Has Audio
- GK
Grace E. Kim, MD
The University of Chicago Medical Center
Chicago, Illinois
Presenting Author(s)
Grace E. Kim, MD1, Mary Rinella, MD2
1The University of Chicago Medical Center, Chicago, IL; 2University of Chicago Medical Center, Chicago, IL
Introduction: Budd-Chiari syndrome (BCS), resulting from obstruction of hepatic venous outflow, is quite rare (reported incidence varies 0.1-10 per million). The most common underlying etiologies in BCS are myeloproliferative disease, e.g. polycythemia vera and essential thrombocytosis, and less commonly, inherited thrombophilia e.g. Factor V Leiden deficiency. BCS associated with sickle cell disease (SSD) is extremely rare with case rare reports in the setting of pronounced symptoms. Here we describe a patient with SSD and hepatomegaly found to have incidental BCS.
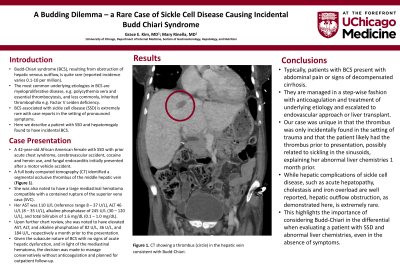
Case Description/Methods: A 42-year-old African American female with SSD with prior acute chest syndrome, cerebrovascular accident, cocaine and heroin use, and fungal endocarditis initially presented after a motor vehicle accident. A full body computed tomography (CT) identified a segmental occlusive thrombus of the middle hepatic vein (Figure 1). She was also noted to have a large mediastinal hematoma compatible with a contained rupture of the superior vena cava (SVC). Her AST was 110 U/L (reference range 8 – 37 U/L), ALT 46 U/L (8 – 35 U/L), alkaline phosphatase of 245 U/L (30 – 120 U/L), and total bilirubin of 1.6 mg/dL (0.1 – 1.0 mg/dL). Upon further chart review, she was noted to have elevated AST, ALT, and alkaline phosphatase of 82 U/L, 36 U/L, and 184 U/L, respectively a month prior to the presentation. Given the subacute nature of BCS with no signs of acute hepatic dysfunction, the decision was made to manage conservatively, without anticoagulation, in light of the in the setting of the mediastinal hematoma, with a plan for outpatient follow-up.
Discussion: Typically, patients with BCS present with abdominal pain or signs of decompensated cirrhosis. They are managed in a step-wise fashion with anticoagulation and treatment of underlying etiology and escalated to endovascular approach or liver transplant. Our case was unique in that the thrombus was only incidentally found in the setting of trauma and that the patient likely had the thrombus prior to presentation, possibly related to sickling in the sinusoids, explaining her abnormal liver chemistries 1 month prior. While hepatic complications of sickle cell disease, such as acute hepatopathy, cholestasis and iron overload are well reported, hepatic outflow obstruction, as demonstrated here, is extremely rare. This highlights the importance of considering Budd-Chiari in the differential when evaluating the patient with SSD and abnormal liver chemistries, even in the absence of symptoms.

Disclosures:
Grace E. Kim, MD1, Mary Rinella, MD2. E0589 - A Budding Dilemma: A Rare Case of Sickle Cell Disease Causing Incidental Budd-Chiari Syndrome, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1The University of Chicago Medical Center, Chicago, IL; 2University of Chicago Medical Center, Chicago, IL
Introduction: Budd-Chiari syndrome (BCS), resulting from obstruction of hepatic venous outflow, is quite rare (reported incidence varies 0.1-10 per million). The most common underlying etiologies in BCS are myeloproliferative disease, e.g. polycythemia vera and essential thrombocytosis, and less commonly, inherited thrombophilia e.g. Factor V Leiden deficiency. BCS associated with sickle cell disease (SSD) is extremely rare with case rare reports in the setting of pronounced symptoms. Here we describe a patient with SSD and hepatomegaly found to have incidental BCS.
Case Description/Methods: A 42-year-old African American female with SSD with prior acute chest syndrome, cerebrovascular accident, cocaine and heroin use, and fungal endocarditis initially presented after a motor vehicle accident. A full body computed tomography (CT) identified a segmental occlusive thrombus of the middle hepatic vein (Figure 1). She was also noted to have a large mediastinal hematoma compatible with a contained rupture of the superior vena cava (SVC). Her AST was 110 U/L (reference range 8 – 37 U/L), ALT 46 U/L (8 – 35 U/L), alkaline phosphatase of 245 U/L (30 – 120 U/L), and total bilirubin of 1.6 mg/dL (0.1 – 1.0 mg/dL). Upon further chart review, she was noted to have elevated AST, ALT, and alkaline phosphatase of 82 U/L, 36 U/L, and 184 U/L, respectively a month prior to the presentation. Given the subacute nature of BCS with no signs of acute hepatic dysfunction, the decision was made to manage conservatively, without anticoagulation, in light of the in the setting of the mediastinal hematoma, with a plan for outpatient follow-up.
Discussion: Typically, patients with BCS present with abdominal pain or signs of decompensated cirrhosis. They are managed in a step-wise fashion with anticoagulation and treatment of underlying etiology and escalated to endovascular approach or liver transplant. Our case was unique in that the thrombus was only incidentally found in the setting of trauma and that the patient likely had the thrombus prior to presentation, possibly related to sickling in the sinusoids, explaining her abnormal liver chemistries 1 month prior. While hepatic complications of sickle cell disease, such as acute hepatopathy, cholestasis and iron overload are well reported, hepatic outflow obstruction, as demonstrated here, is extremely rare. This highlights the importance of considering Budd-Chiari in the differential when evaluating the patient with SSD and abnormal liver chemistries, even in the absence of symptoms.

Figure: Figure 1. Computed tomography (CT) showing a segmental occlusive thrombus of the middle hepatic vein.
Disclosures:
Grace Kim indicated no relevant financial relationships.
Mary Rinella indicated no relevant financial relationships.
Grace E. Kim, MD1, Mary Rinella, MD2. E0589 - A Budding Dilemma: A Rare Case of Sickle Cell Disease Causing Incidental Budd-Chiari Syndrome, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
