Back

Poster Session B - Monday Morning
Category: General Endoscopy
B0292 - Differentiating CMV Colitis From GVHD in Post-Transplant Patients: A Case Study
Monday, October 24, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom
Has Audio

Rafeh Safdar, MBBS
Albany Medical Center
Albany, NY
Presenting Author(s)
Rafeh Safdar, MBBS, Momina Amjad, MBBS, Sualeha Khalid, MBBS, Mihir Raval, MD, MPH
Albany Medical Center, Albany, NY
Introduction: Cytomegalovirus (CMV) infection can complicate the clinical course of immunocompromised patients including allogeneic hematopoietic stem cell transplant (allo-HSCT) recipients, where the infection can be serious. CMV can involve different organs including lungs, brain, eyes, and the GI tract. Signs and symptoms of CMV infection may overlap with other conditions including graft-versus-host disease (GVHD), a multisystem disorder commonly seen in allo-HSCT recipients.
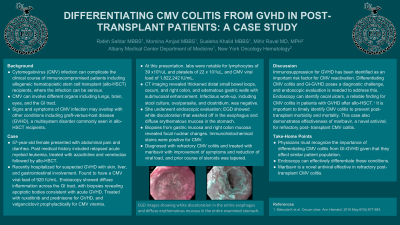
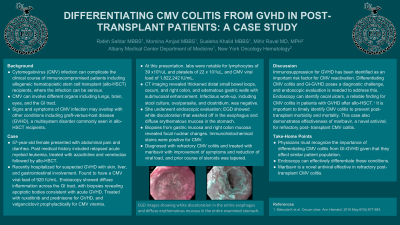
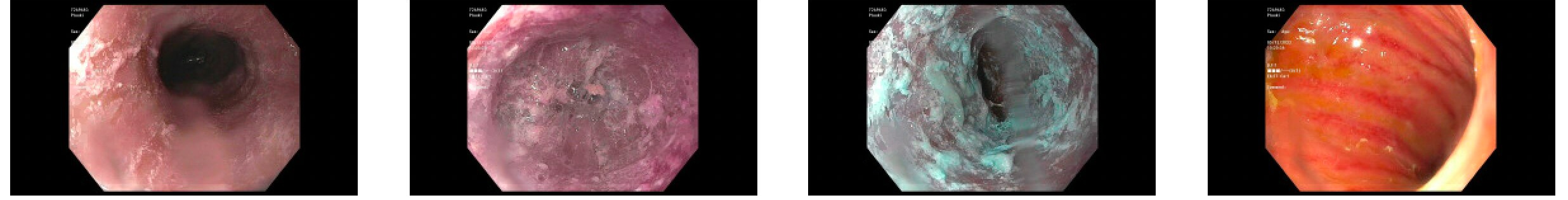
Case Description/Methods: A 57-year-old female presented with abdominal pain and diarrhea. Past medical history included relapsed acute myeloid leukemia, treated with azacitidine and venetoclax followed by allo-HSCT. She was recently hospitalized for suspected GVHD with skin, liver, and gastrointestinal involvement. She was also found to have a CMV viral load of 920 IU/mL. Endoscopy showed diffuse inflammation across the GI tract, with biopsies revealing apoptotic bodies consistent with acute GVHD. She was treated with ruxolitinib and prednisone for GVHD, and valganciclovir prophylactically for CMV viremia. At this presentation, labs were notable for lymphocytes of 39 x103/uL and platelets of 22 x 103/uL, and CMV viral load of 1,822,242 IU/mL. CT imaging revealed thickened distal small bowel loops, cecum, and right colon, and edematous gastric walls with submucosal enhancement. Infectious work-up, including stool culture, ova/parasite, and clostridium, was negative. She underwent endoscopic evaluation; EGD showed white discoloration that washed off in the esophagus and diffuse erythematous mucosa in the stomach. Biopsies from gastric mucosa and right colon mucosa revealed focal nuclear changes. Immunohistochemical stains were positive for CMV. She was diagnosed with refractory CMV colitis and treated with maribavir with improvement of symptoms and reduction of viral load, and prior course of steroids was tapered.
Discussion: Immunosuppression for GVHD has been identified as an important risk factor for CMV reactivation. Differentiating CMV colitis and GI-GVHD poses a diagnostic challenge, and endoscopic evaluation is needed to address this. Endoscopy can identify cecal ulcers, a reliable finding for CMV colitis in patients with GVHD after allo-HSCT.1 It is important to timely identify CMV colitis to prevent post-transplant morbidity and mortality. This case also demonstrates effectiveness of maribavir, a novel antiviral, for refractory post-transplant CMV colitis.
1. Matsuda K et al. Cecum ulcer. Ann Hematol. 2018 May;97(5):877-883.
Disclosures:
Rafeh Safdar, MBBS, Momina Amjad, MBBS, Sualeha Khalid, MBBS, Mihir Raval, MD, MPH. B0292 - Differentiating CMV Colitis From GVHD in Post-Transplant Patients: A Case Study, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
Albany Medical Center, Albany, NY
Introduction: Cytomegalovirus (CMV) infection can complicate the clinical course of immunocompromised patients including allogeneic hematopoietic stem cell transplant (allo-HSCT) recipients, where the infection can be serious. CMV can involve different organs including lungs, brain, eyes, and the GI tract. Signs and symptoms of CMV infection may overlap with other conditions including graft-versus-host disease (GVHD), a multisystem disorder commonly seen in allo-HSCT recipients.
Case Description/Methods: A 57-year-old female presented with abdominal pain and diarrhea. Past medical history included relapsed acute myeloid leukemia, treated with azacitidine and venetoclax followed by allo-HSCT. She was recently hospitalized for suspected GVHD with skin, liver, and gastrointestinal involvement. She was also found to have a CMV viral load of 920 IU/mL. Endoscopy showed diffuse inflammation across the GI tract, with biopsies revealing apoptotic bodies consistent with acute GVHD. She was treated with ruxolitinib and prednisone for GVHD, and valganciclovir prophylactically for CMV viremia. At this presentation, labs were notable for lymphocytes of 39 x103/uL and platelets of 22 x 103/uL, and CMV viral load of 1,822,242 IU/mL. CT imaging revealed thickened distal small bowel loops, cecum, and right colon, and edematous gastric walls with submucosal enhancement. Infectious work-up, including stool culture, ova/parasite, and clostridium, was negative. She underwent endoscopic evaluation; EGD showed white discoloration that washed off in the esophagus and diffuse erythematous mucosa in the stomach. Biopsies from gastric mucosa and right colon mucosa revealed focal nuclear changes. Immunohistochemical stains were positive for CMV. She was diagnosed with refractory CMV colitis and treated with maribavir with improvement of symptoms and reduction of viral load, and prior course of steroids was tapered.
Discussion: Immunosuppression for GVHD has been identified as an important risk factor for CMV reactivation. Differentiating CMV colitis and GI-GVHD poses a diagnostic challenge, and endoscopic evaluation is needed to address this. Endoscopy can identify cecal ulcers, a reliable finding for CMV colitis in patients with GVHD after allo-HSCT.1 It is important to timely identify CMV colitis to prevent post-transplant morbidity and mortality. This case also demonstrates effectiveness of maribavir, a novel antiviral, for refractory post-transplant CMV colitis.
1. Matsuda K et al. Cecum ulcer. Ann Hematol. 2018 May;97(5):877-883.
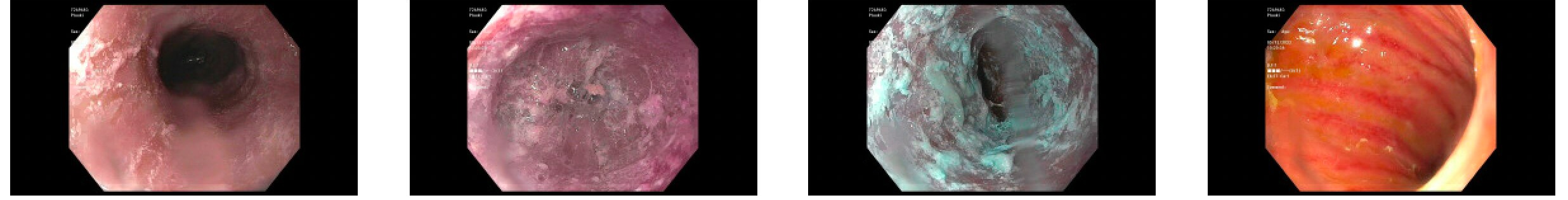
Figure: EGD images showing white discoloration in the entire esophagus and diffuse erythematous mucosa in the entire examined stomach.
Disclosures:
Rafeh Safdar indicated no relevant financial relationships.
Momina Amjad indicated no relevant financial relationships.
Sualeha Khalid indicated no relevant financial relationships.
Mihir Raval indicated no relevant financial relationships.
Rafeh Safdar, MBBS, Momina Amjad, MBBS, Sualeha Khalid, MBBS, Mihir Raval, MD, MPH. B0292 - Differentiating CMV Colitis From GVHD in Post-Transplant Patients: A Case Study, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
