Back

Poster Session E - Tuesday Afternoon
Category: Small Intestine
E0651 - A Unique Case of Progressive Disseminated Histoplasmosis With Significant Gastrointestinal Involvement
Tuesday, October 25, 2022
3:00 PM – 5:00 PM ET
Location: Crown Ballroom
Has Audio

Neil Khoury, MD
NYP Brooklyn Methodist Hospital
Brooklyn, NY
Presenting Author(s)
Neil Khoury, MD1, Ranbir Singh, MD1, Dean Rizzi, MD2, Michael Castillo, MD3, Shah Giashuddin, MD1, Ilan Weisberg, MD1
1NYP Brooklyn Methodist Hospital, Brooklyn, NY; 2New York Presbyterian Brooklyn Methodist, Brooklyn, NY; 3New York Presbyterian Brooklyn Methodist Hospital, Brooklyn, NY
Introduction: Histoplasmosis is a predominantly pulmonary fungal infection, caused by inhalation of Histoplasma Capsulatum. Immunocompetent individuals typically have self-limiting disease, while immunosuppressed individuals are at risk for severe disease complications, including extrapulmonary manifestations. We present a rare case of a transgender woman with disseminated histoplasmosis complicated by severe gastrointestinal manifestations including small bowel obstruction, splenic infarction, hepatopathy, ileitis and large colonic masses.
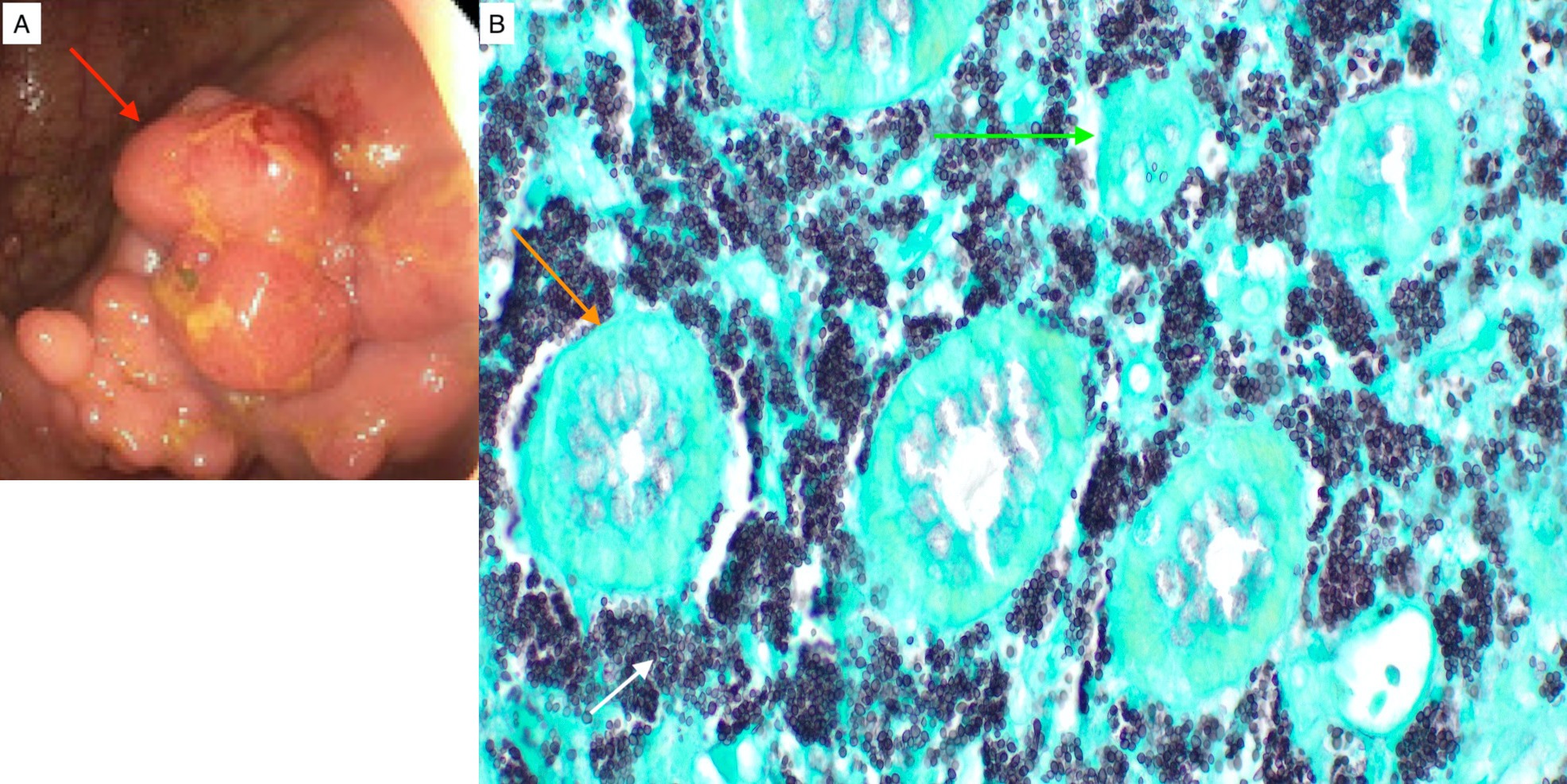
Case Description/Methods: A 43-year-old transgender woman with AIDS was first identified to have disseminated histoplasmosis in a bone marrow biopsy done in 2018 for anemia. Since then, her long history of medication noncompliance had resulted in diffuse gastrointestinal manifestations. In 2019, she developed a small bowel obstruction due to excessive fungal infiltration of Peyer’s patches. She underwent an exploratory laparotomy and partial small bowel resection with primary anastomosis and splenectomy due to an incidentally noted splenic infarct on abdominal CT. Spleen pathology revealed extensive necrosis, as well as positive GMS and PAS stains for fungal budding yeasts within histiocytes. Amphotericin infusions with eventual transition to maintenance oral itraconazole dosing led to initial suppression of her infection, until the latter was no longer covered by her insurance. In early 2022, after being off of antifungal treatment for about two months, a repeat colonoscopy revealed multiple large, polypoid, non-obstructing cecal masses (Figure 1). Pathology reports revealed histiocytic aggregates (GMS+, PAS+), and she was restarted on 4-6 weeks of IV amphotericin.
Discussion: This unique case emphasizes the varied GI manifestations of disseminated histoplasmosis and emphasizes the importance of access to care. It is important to keep this atypical presentation in mind as clinical improvement is often achieved with prompt antifungal treatment. However, recurrence is seen in 50% of patients, despite adherence to therapy. As a member of the LGBTQ community, our patient has well known personal and institutional barriers to healthcare. It is unclear if her recurrence was from failed therapy or due to barriers in consistent care. If left untreated, disseminated histoplasmosis has a mortality rate of >90% within one year. Thus, it is imperative to identify patients with potential barriers to health care to reduce morbidity and mortality.
Disclosures:
Neil Khoury, MD1, Ranbir Singh, MD1, Dean Rizzi, MD2, Michael Castillo, MD3, Shah Giashuddin, MD1, Ilan Weisberg, MD1. E0651 - A Unique Case of Progressive Disseminated Histoplasmosis With Significant Gastrointestinal Involvement, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1NYP Brooklyn Methodist Hospital, Brooklyn, NY; 2New York Presbyterian Brooklyn Methodist, Brooklyn, NY; 3New York Presbyterian Brooklyn Methodist Hospital, Brooklyn, NY
Introduction: Histoplasmosis is a predominantly pulmonary fungal infection, caused by inhalation of Histoplasma Capsulatum. Immunocompetent individuals typically have self-limiting disease, while immunosuppressed individuals are at risk for severe disease complications, including extrapulmonary manifestations. We present a rare case of a transgender woman with disseminated histoplasmosis complicated by severe gastrointestinal manifestations including small bowel obstruction, splenic infarction, hepatopathy, ileitis and large colonic masses.
Case Description/Methods: A 43-year-old transgender woman with AIDS was first identified to have disseminated histoplasmosis in a bone marrow biopsy done in 2018 for anemia. Since then, her long history of medication noncompliance had resulted in diffuse gastrointestinal manifestations. In 2019, she developed a small bowel obstruction due to excessive fungal infiltration of Peyer’s patches. She underwent an exploratory laparotomy and partial small bowel resection with primary anastomosis and splenectomy due to an incidentally noted splenic infarct on abdominal CT. Spleen pathology revealed extensive necrosis, as well as positive GMS and PAS stains for fungal budding yeasts within histiocytes. Amphotericin infusions with eventual transition to maintenance oral itraconazole dosing led to initial suppression of her infection, until the latter was no longer covered by her insurance. In early 2022, after being off of antifungal treatment for about two months, a repeat colonoscopy revealed multiple large, polypoid, non-obstructing cecal masses (Figure 1). Pathology reports revealed histiocytic aggregates (GMS+, PAS+), and she was restarted on 4-6 weeks of IV amphotericin.
Discussion: This unique case emphasizes the varied GI manifestations of disseminated histoplasmosis and emphasizes the importance of access to care. It is important to keep this atypical presentation in mind as clinical improvement is often achieved with prompt antifungal treatment. However, recurrence is seen in 50% of patients, despite adherence to therapy. As a member of the LGBTQ community, our patient has well known personal and institutional barriers to healthcare. It is unclear if her recurrence was from failed therapy or due to barriers in consistent care. If left untreated, disseminated histoplasmosis has a mortality rate of >90% within one year. Thus, it is imperative to identify patients with potential barriers to health care to reduce morbidity and mortality.
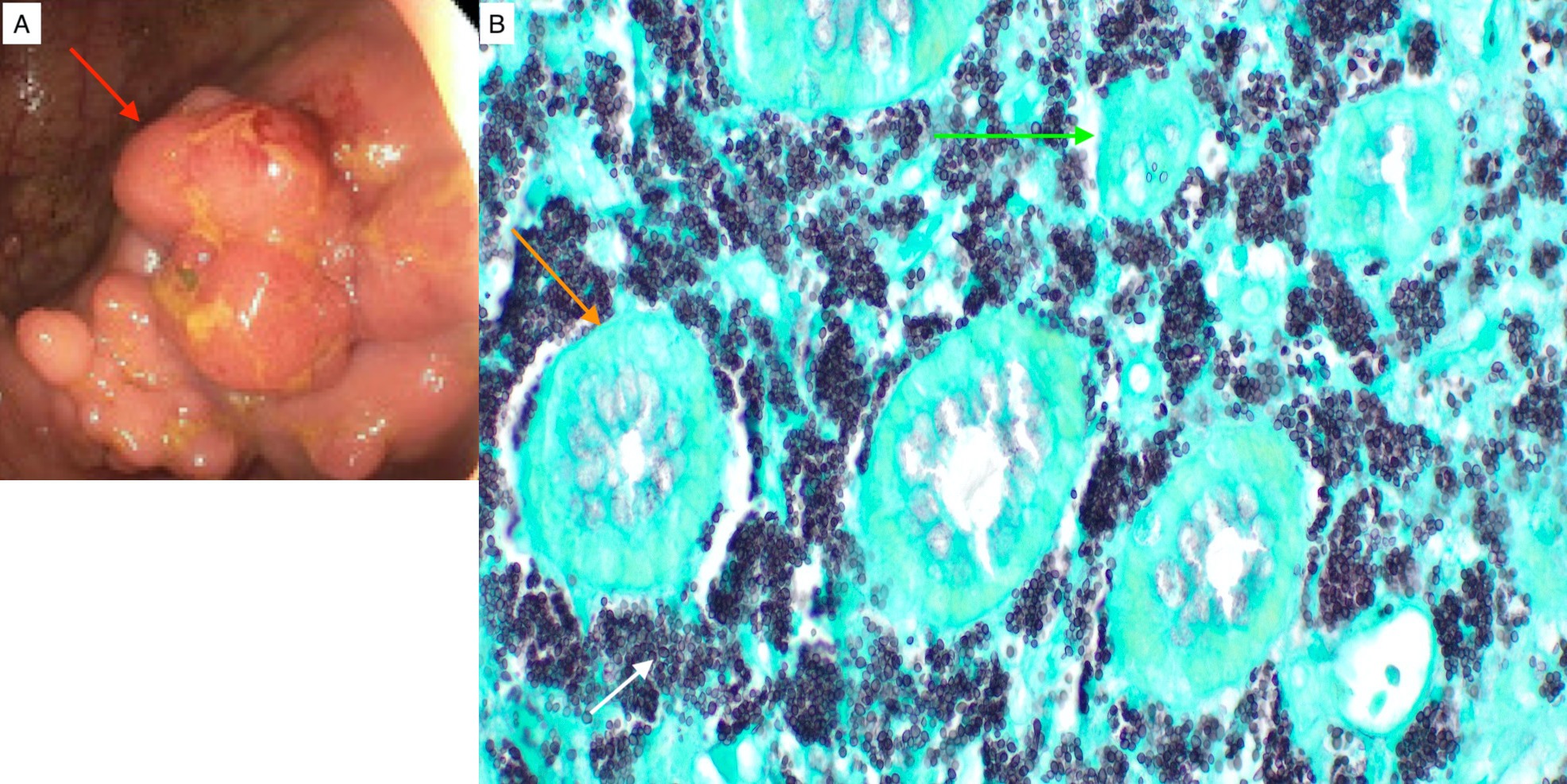
Figure: Figure A: Polypoid histoplasmosis mass found in cecum on colonoscopy (Red Arrow)
Figure B: Histology slide of the terminal ileum biopsy using GMS stain. Intestinal crypts of the ileum (orange arrow) are surrounded by densely packed Histoplasma capsulatum (white arrow). Some crypts are formed while others appeared destroyed by this fungus (green arrow).
Figure B: Histology slide of the terminal ileum biopsy using GMS stain. Intestinal crypts of the ileum (orange arrow) are surrounded by densely packed Histoplasma capsulatum (white arrow). Some crypts are formed while others appeared destroyed by this fungus (green arrow).
Disclosures:
Neil Khoury indicated no relevant financial relationships.
Ranbir Singh indicated no relevant financial relationships.
Dean Rizzi indicated no relevant financial relationships.
Michael Castillo indicated no relevant financial relationships.
Shah Giashuddin indicated no relevant financial relationships.
Ilan Weisberg indicated no relevant financial relationships.
Neil Khoury, MD1, Ranbir Singh, MD1, Dean Rizzi, MD2, Michael Castillo, MD3, Shah Giashuddin, MD1, Ilan Weisberg, MD1. E0651 - A Unique Case of Progressive Disseminated Histoplasmosis With Significant Gastrointestinal Involvement, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
